Drug design to target cancer and inflammatory disease
Chemists at Indiana University Bloomington have produced detailed descriptions of the structure and molecular properties of human folate receptor proteins, a key development for designing new drugs that can target cancer and inflammatory diseases without serious side effects.
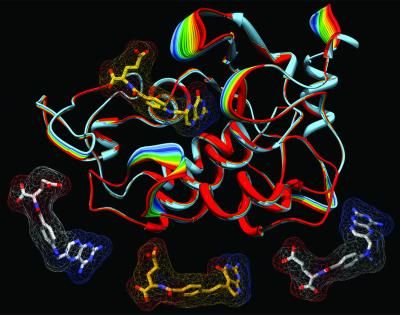
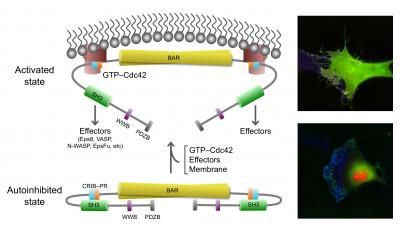
This image shows models of the human folate receptor (top) and antifolate drugs used in chemotherapy (bottom, from left: aminopterin, pemetrexed and methotrexate).
Charles Dann III, Indiana University
The researchers, from the lab of Charles Dann III, assistant professor of chemistry in the College of Arts and Sciences, published their findings in the Proceedings of the National Academy of Sciences. Dann said the results should help chemists create more effective antifolate drugs, which act by interfering with the ability of folates -- also called folic acid or vitamin B9 -- to perform tasks that are essential for cell growth.
The findings could be especially helpful against epithelial cell cancers, including ovarian cancers that are resistant to treatment and nearly always fatal. They could also guide the design of drugs for inflammatory diseases such as rheumatoid arthritis, Crohn's disease and psoriasis.
Physicians have used antifolates for 60 years to treat cancer, and the drugs are often effective at killing cancer cells. The problem is, they aren't selective.
"The antifolates that are currently available also enter normal, healthy cells and kill those as well," Dann said. "What we're describing is an entryway into cancer cells that can be exploited to specifically target or attack cancer cells with drugs.
One reason for the multiple chemotherapeutic side effects of current antifolates is that they typically enter cells via routes that are present in most cell types, not just in cancer cells. The PNAS paper, on the other hand, examines the potential for targeting a different entry route in which the molecules bind with human folate receptors, which are widely present in certain cancer cells and in causal cells of inflammatory disease, but not in normal cells.
Dann describes the folate receptors as "locks" that can be used to open a door into the cell. By gaining a better understanding of what the lock looks like and how it works, researchers can build a better key -- that is, a better antifolate drug -- to open the door.
The lab does this by taking "molecular snapshots" of the folate receptor proteins, capturing the placement of atoms and the origami-like twists and folds of the molecules to reveal how folates and antifolates are likely to bind with the molecules. To understand the structures, the researchers must first convert the receptor proteins to crystals, a complex task that was helped greatly by using the Crystallization Automation Facility in Simon Hall, a recent project of IU's MetaCyt initiative that allows high-throughput crystallography of proteins using advanced robotics.
"The goal is to hit those cells that are causative of disease but not hit the normal cells," Dann said. "For decades, antifolates were all we had for treating certain cancers. Antifolates are great, but we think they can be made better by targeting them to specific cells."
The researchers describe six models to show how antifolates bind with the folate receptors and to examine "biological trafficking" mechanisms that introduce antifolates into cells. The models include the folate receptor in three distinct stages of trafficking and in combination with three antifolates that have been used in clinical settings: pemetrexed, aminopterin and methotrexate.
Dann said evidence suggests the antifolate drugs that have been used to date can bind with the folate receptors but aren't effectively released into the cells -- in effect, the key fits into and jams the lock, making entry impossible. The three-dimensional models of folate receptor proteins should help drug designers create medications that will target, enter and kill cancer cells.