A new era of allergy treatment
Scientists unveil the early molecular key to curing life-threatening allergies
Advertisement
In a landmark clinical study just published in Nature Communications, researchers from the Luxembourg Institute of Health (LIH), the Luxembourg Centre for Systems Biomedicine (LCSB) of the University of Luxembourg, the Allergy Center Wiesbaden, Ulm University Hospital and the Brussels Vrije Universiteit revealed the early immune mechanisms behind the exceptional success of insect venom Immunotherapy. The study identified early molecular and cellular changes already at 8 hours immediately following the first immunotherapy administrations, changes that will pave the way for curative immune tolerance. Overall it provides novel insights that could revolutionise allergy treatment and improve outcomes for millions suffering from chronic immune disorders.
Allergic diseases are rapidly increasing globally, becoming the most common chronic immune-mediated conditions, largely driven by modern lifestyle factors and environmental influences. While allergen-specific immunotherapy (AIT) is the only available treatment that can potentially cure certain allergies, its effectiveness varies greatly among various forms of allergies. Insect venom allergies—such as those caused by bee or wasp stings—are the exception, with AIT offering clinical cure rates exceeding 90-95%.
A new study by the Luxembourg Institute of Health (LIH), in collaboration with the Centre Hospitalier de Luxembourg (CHL), the Allergy Center Wiesbaden, Ulm University Hospital and the Brussels Vrije Universiteit, shed light on the early immune mechanisms that underpin this remarkably successful therapy. By exploring how the immune system develops long-term tolerance to insect venom, the clinical research study identified key molecular and cellular switches that occur in the early stages of treatment, providing hope for improving AIT against other allergic diseases, where AIT is less successful, and contributing to the broader effort to combat the global allergy epidemic.
“This work is a breakthrough for allergy science,” explained co-first author of the study Prof Sebastian Bode, jointly affiliated to the Luxembourg Institute of Health Department of Infection and Immunity (DII), the Ulm University Medical Center Department of Pediatrics and Adolescent Medicine, and the Department of General Pediatrics, Adolescent Medicine and Neonatology, Medical Centre–University of Freiburg, Germany. “We’ve uncovered early immune responses, including the regulation of IL-6—a molecule usually linked to inflammation—that might play a completely unexpected crucial role in restoring immune tolerance. These findings could guide the development of more effective treatments for other allergies.”
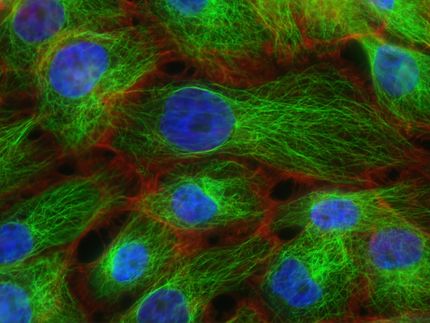
The study involved over 200 blood samples from patients recruited and treated at CHL by a team of allergy specialists, which then underwent detailed analysis at LIH’s Department of Infection and Immunity (DII), the Integrated BioBank of Luxembourg (IBBL), and the Luxembourg Centre for Systems Biomedicine (LCSB). This represents the deepest and most comprehensive data analysis ever performed in patients with insect sting allergy, which affects roughly 2.6%-4% of the population in Europe and worldwide—approximately 13-20 million people across the EU and UK—who are at risk of a fatal outcome from an insect sting if not treated by insect venom AIT. International collaborators from the VUB University Hospital in Brussels and Allergy Centre Wiesbaden in Germany provided additional expertise, ensuring a thorough and wide-reaching investigation.
“The scope and precision of this study are unparalleled,” noted Professor Jorge Goncalves, a computational expert at the Luxembourg Centre for Systems Biomedicine, University of Luxembourg. “We developed advanced algorithms to enable the analyses of the massive datasets of >200 millions of immune cells, which otherwise could not be handled at all by previously existing approaches.”
“We unbiasedly analysed each of the 25,000 genes in a pathogenic T-cell subset purified from ~ 200 blood samples,” added Assistant Professor Enrico Glaab, a big-data scientist, also from the Luxembourg Centre for Systems Biomedicine, “Our novel tools have accelerated data processing, allowing us to uncover the hidden early molecular mechanisms driving immune tolerance.”
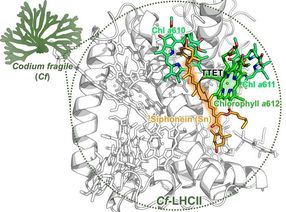
“One of the study’s most revolutionary findings was the discovery of a controlled, low-level activation of the IL-6 pathway within a specific immune subset during allergen-specific immunotherapy (AIT) for insect venom allergies,” said Dr Feng Hefeng, one of the study’s co-senior authors. “While IL-6 is typically known for driving inflammation in chronic diseases, our research revealed its unexpected role in the immune system’s transition to tolerance. We found that during AIT, IL-6 is temporally activated at much lower levels than in typical inflammatory responses, playing a crucial protective role. This subtle but crucial activation helps the body adapt to venom allergens, promoting long-term immune tolerance and preventing severe allergic reactions.”
The research also highlighted the importance of B regulatory cells (Bregs) very early during AIT, which are vital by producing IL-10 for maintaining immune system balance in many diseases. Additionally, the study identified specific hybrid plastic immune cells that combine features of several well-known classical immune subsets. These hybrid cells play a key role in bridging the innate and adaptive immune responses, facilitating the immune system’s transition to tolerance. The discovery of these flexible immune cells offers new insights into the “molecular magic” behind insect venom AIT.
“Allergic diseases are the most common chronic immune-mediated conditions globally, affecting millions,” said Prof Ludger Klimek from the German Center for Rhinology and Allergology. “By understanding why insect venom AIT is so effective, we hope to improve therapies for other allergens and ultimately combat the growing allergy epidemic.”
In addition to its scientific contributions, the study has practical implications. It demonstrates the necessity of considering circadian rhythms when designing clinical studies, as immune responses fluctuate throughout the day. The findings have also inspired the creation of an interactive immune data platform that is directly linked to the publication and allows researchers worldwide to explore the study’s results and use them as a foundation for further research.
“This is translational research at its finest,” added Professor Jan Gutermuth, from the Department of Dermatology, Vrije Universiteit Brussel. “Our work bridges clinical practice and cutting-edge science, using insect venom immunotherapy as a clinical model to unlock the secrets of immune tolerance. The potential to transform allergy treatments is immense.”
“The findings are expected to have far-reaching implications, not only for improving allergy treatments but also for understanding immune tolerance in other chronic conditions. By unravelling the “molecular magic” of insect venom immunotherapy, researchers are one step closer to addressing the global allergy epidemic and advancing personalised medicine,” concluded Professor Markus Ollert, lead author of the work and Director of the LIH Department of Infection and Immunity.
Original publication
Dimitrii Pogorelov, Sebastian Felix Nepomuk Bode, Xin He, Javier Ramiro-Garcia, Fanny Hedin, Wim Ammerlaan, Maria Konstantinou, Christophe M. Capelle, Ni Zeng, ... Mohamed H. Shamji, Fay Betsou, Paul Wilmes, Enrico Glaab, Antonio Cosma, Jorge Goncalves, Feng Q. Hefeng, Markus Ollert; "Multiomics approaches disclose very-early molecular and cellular switches during insect-venom allergen-specific immunotherapy: an observational study"; Nature Communications, Volume 15, 2024-11-26