Precision with stem cells a step forward for treating MS, other diseases
Scientists have improved upon their own previous world-best efforts to pluck out just the right stem cells to address the brain problem at the core of multiple sclerosis and a large number of rare, fatal children's diseases.
Details of how scientists isolated and directed stem cells from the human brain to become oligodendrocytes – the type of brain cell that makes myelin, a crucial fatty material that coats neurons and allows them to signal effectively – were published in Nature Biotechnology by scientists at the University of Rochester Medical Center and the University at Buffalo.
Scientists injected the cells into the brains of mice that were born without the ability to make myelin. Twelve weeks later, the cells had become oligodendrocytes and had coated more than 40 percent of the brain's neurons with myelin – a four-fold improvement over the team's previous results published in Cell Stem Cell and Nature Medicine.
"These cells are our best candidates right now for someday helping patients with M.S., or children with fatal hereditary myelin disorders," said Steven Goldman, M.D., Ph.D., the leader of the team and professor and chair of the Department of Neurology at the University of Rochester Medical Center. "These cells migrate more effectively throughout the brain, and they myelinate other cells more quickly and more efficiently than any other cells assessed thus far. Now we finally have a cell type that we think is safe and effective enough to propose for clinical trials."
The first author and co-corresponding author of the paper is Fraser Sim, Ph.D., assistant professor of Pharmacology and Toxicology at the University at Buffalo, who did much of the work while he was a researcher at Rochester.
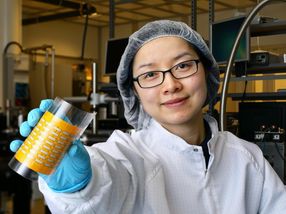
Sim and Rochester graduate student Crystal McClain ran extensive analyses looking at gene activity in different types of stem cells, leading to the conclusion that stem cells carrying a protein known as CD140a on their surface seemed to be most likely to become the desired cells – oligodendrocytes.
"Characterizing and isolating the exact cells to use in stem cell therapy is one key to ultimately having success," said Sim. "You need to have the right cells in hand before you can even think about getting to a clinical trial to treat people. This is a significant step."
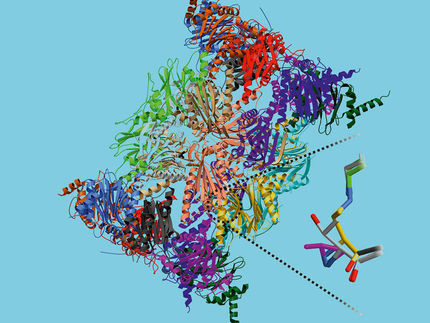
Central to the team's success is its encyclopedic knowledge of the hundreds of molecules that direct brain stem cells to become the specific cell types of the adult brain. That knowledge is the product of a decade of work in the Goldman lab.
In the experiments described in Nature Biotechnology, for instance, the team was able to use a molecule called BMP4 to direct the stem cells to become support cells of the brain – astrocytes – while another molecule called Noggin led them to become oligodendrocytes.
"These cells are very responsive to cues in their local environment," said Goldman. "It's crucial to select the right type of stem cell, but it's just as important to create an environment with the molecular signals necessary to produce the type of cell needed for a particular condition or illness."
The current work focuses on the creation of myelin; besides it loss in multiple sclerosis and childhood disorders, myelin loss plays a role in diseases as diverse as cerebral palsy, diabetes, high blood pressure, and some cases of stroke. While Goldman's team has had previous success remyelinating the brains of mice born without the substance, the new results identify a specific subset of cells that appear to be the most efficient yet at producing myelin and improve the hope of developing cell therapy as a way to treat these diseases.
An eventual treatment of a disease like M.S. might involve injecting stem cells to create myelin in the brains of patients. Along those lines, Martha Windrem, Ph.D., an author of the paper and assistant professor in Rochester's Department of Neurology, has developed methods to inject cells in such a way that they migrate throughout a large swath of the brain, laying down myelin on neurons as they go.
"Another approach," says Sim, "might involve using certain medications to turn on these cells already present in the brains of patients and thereby create new myelin. The use of the new techniques described in this work will permit us to better understand how human cells behave in the brain and help us predict which medications may be successful in the treatment of myelin loss."