The armorers: How dendritic cells activate the immune system
Thanks to this “armoring function”, dendritic cells constitute a ray of hope for personalized immunotherapy
As part of the immune system, dendritic cells are essential for fighting body cells that have degenerated or are infected with a virus. They trigger an immune response by presenting protein fragments, for example of viruses, to T cells. In so doing, they activate the latter so that these recognize the fragments as foreign. Certain membrane proteins, MHC-I molecules, enable this process within dendritic cells. Researchers at Goethe University Frankfurt and its partner institutes have now identified further interaction partners of the protein complex responsible for loading MHC-I molecules in dendritic cells.
The specific or acquired immune system of vertebrates is a powerful weapon against pathogens and pathologically altered body cells. Here, T cells play a special role. After activation, they can systematically kill off target cells that have degenerated or are infected with a virus. They carry a receptor on their surface that recognizes small protein fragments – antigens – presented to them by specialized immune cells, including the highly efficient dendritic cells. These are phagocytes (scavenger cells) that patrol through the body in search of infected or degenerated cells, ingest them and degrade them inside a membrane vesicle. During this process, antigens are produced that enable the dendritic cells to bind to MHC-I receptors and then present them on the cell surface.
The antigenic MHC-I molecules remain stable for several days. During this time, their purpose is to activate immature (naïve) T cells and transform them into potent killer cells (cytotoxic T cells). Thanks to this “armoring function”, dendritic cells constitute a ray of hope for personalized immunotherapy. With the participation of Dr. Christian Schölz from the Max von Pettenkofer Institute in Munich as well as Professor Reinhold Förster and Professor Ulrich Kalinke from Hannover Medical School, a team led by Professor Robert Tampé from Goethe University Frankfurt has now been able to show that the protein complex responsible for loading MHC-I molecules in dendritic cells is organized in supramolecular assemblies for particularly efficient antigen presentation.
Like all surface proteins, MHC-I molecules are incorporated into the membrane of the intracellular endoplasmic reticulum (ER) during synthesis. The ER is a system of tubules and sacs inside the cell, in which the MHC-I molecules are loaded with antigens carried there via a transporter called TAP.
Small vesicles with the loaded MHC-I molecules bud off from the endoplasmic reticulum, migrate to the cell membrane and fuse with it so that they appear on the cell surface and can interact with T cells. “All body cells with a nucleus present their own antigens to the immune system,” Tampé explains, “but dendritic cells are the ones that present the antigens of other cells on MHC-I best of all and in this way are able to arm T cells.” This is because dendritic cells have an ER with a particularly extensive network of tubules and sacs.
For their experiments, the researchers examined dendritic cells in an early stage of cell development, known as progenitor cells, allowing them to develop first into immature and then mature dendritic cells. In all three groups of cells, they found an antigenic peptide loading complex composed of TAP, MHC-I and three other proteins: tapasin, ERp57 and calreticulin, folding enzymes (chaperones) that help the three-dimensional structure of MHC-I to form correctly.
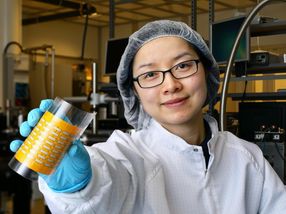
In the mature dendritic cells, three other proteins further enriched the loading complex: The researchers discovered VAPA and ESYT1 in close proximity, which normally appear at contact sites between the ER and other cell membranes, as well as BAP31. BAP31 occurs at ER exit sites, that is, where the vesicles with the folded proteins bud off from the ER. “This result indicates that antigen processing in dendritic cells is more efficient when the loading complex does not operate on its own but works in organized alliances,” says Martina Barends, one of the first authors of the research paper.
This cooperation with the newly described partners suggests that loading of MHC-I molecules occurs at ER exit sites, which could enable the complexes to reach the cell surface particularly quickly. Moreover, loading complexes at contact sites between the ER and plasma membrane could facilitate direct transport to the cell surface. Tampé is convinced: “This would make antigen presentation far more efficient.” The hope now is that these findings will help in the development of new immunization strategies and immunotherapies. “We now have a better idea of how antigens are produced in dendritic cells that can be used therapeutically,” summarizes Tampé.