Minor Mutations in Avian Flu Virus Increase Chances of Human Infection
Few Adaptations Are Needed to Transform It into a Potential Pandemic Virus
Advertisement
Scientists at The Scripps Research Institute, the Centers for Disease Control, and the Armed Forces Institute of pathology have identified what the researchers described as a possible pathway for a particularly virulent strain of the avian flu virus H5N1 "to gain a foothold in the human population."
The H5N1 avian influenza virus, commonly known as "bird flu," is a highly contagious and deadly disease in poultry. So far, its spread to humans has been limited, with 177 documented severe infections, and nearly 100 deaths in Indonesia, Vietnam, Thailand, Cambodia, China, Iraq, and Turkey as of March 14, 2006, according to the World Health Organization.
"With continued outbreaks of the H5N1 virus in poultry and wild birds, further human cases are likely," said Ian Wilson, a Scripps Research professor of molecular biology and head of the laboratory that conducted the recent study. "The potential for the emergence of a human-adapted H5 virus, either by re-assortment or mutation, is a clear threat to public health worldwide."
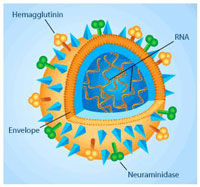
Of the H5N1 strains isolated to date, the researchers looked at A/Vietnam/1203/2004 (Viet04), one of the most pathogenic H5N1 viruses studied so far. The virus was originally isolated from a 10-year-old Vietnamese boy who died from the infection in 2004. The hemagglutinin (HA) structure from the Viet04 virus was found to be closely related to the 1918 virus HA, which caused some 50 million deaths worldwide.
Using a recently developed microarray technology the study showed that relatively small mutations can result in switching the binding site preference of the avian virus from receptors in the intestinal tract of birds to the respiratory tract of humans.These mutations, the study noted, were already "known in [some human influenza] viruses to increase binding for these receptors." The study was published on March 16, 2006 by ScienceXpress, the advance online version of the journal Science.
Receptor specificity for the influenza virus is controlled by the glycoprotein hemagglutinin (HA) on the virus surface. These viral HAs bind to host cell receptors containing complex glycans that in turn contain terminal sialic acids. Avian viruses prefer binding to a2-3-linked sialic acids on receptors of intestinal epithelial cells, while human viruses are usually specific for the a2-6 linkage on epithelial cells of the lungs and upper respiratory tract. Such interactions allow the virus membrane to fuse with the membrane of the host cell so that viral genetic material can be transferred to the cell.
The switch from a2-3 to a2-6 receptor specificity is a critical step in the adaptation of avian viruses to a human host and appears to be one of the reasons why most avian influenza viruses, including current avian H5 strains, are not easily transmitted from human-to-human following avian-to-human infection. However, the report did suggest that "once a foothold in a new host species is made, the virus HA can optimize its specificity to the new host."
"Our recombinant approach to the structural analysis of the Viet04 virus showed that when we inserted HA mutations that had already been shown to shift receptor preference in H3 HAs to the human respiratory tract, the mutations increased receptor preference of the Viet04 HA towards specific human glycans that could serve as receptors on lung epithelial cells," Wilson said. "The effect of these mutations on the Viet04 HA increases the likelihood of binding to and infection of susceptible epithelial cells."
The study was careful to note that these results reveal only one possible route for virus adaptation. The study concluded that other, as yet "unidentified mutations" could emerge, allowing the avian virus to switch receptor specificity and make the jump to human-to-human transmission.