Twin sisters provides clues for battling aggressive cancers
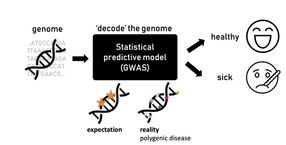
Analyzing the genomes of twin 3-year-old sisters – one healthy and one with aggressive leukemia – led an international team of researchers to identify a novel molecular target that could become a way to treat recurring and deadly malignancies.
Scientists in China and the United States report their findings online in Nature Genetics. The study points to a molecular pathway involving a gene called SETD2, which can mutate in blood cells during a critical step as DNA is being transcribed and replicated.
The findings stem from the uniquely rare opportunity to compare the whole genomes of the monozygotic twin sisters (which means they came from a single egg). This led to a series of follow up experiments in human samples from leukemia patients and mouse models of human disease. Those tests verified and extended initial findings researchers gleaned from the twin sisters' blood samples, according to Gang Huang, PhD, co-corresponding author and a researcher in the divisions of Pathology and Experimental Hematology and Cancer Biology at Cincinnati Children's Hospital Medical Center.
"We reasoned that monozygotic twins discordant for human leukemia would have identical inherited genetic backgrounds and well-matched tissue-specific events," Huang said. "This provided a strong basis for comparison and analysis. We identified a gene mutation involving SETD2 that contributes to the initiation and progression of leukemia by promoting the self-renewal potential of leukemia stem cells."
The twin sisters' genomes were compared at the laboratory of co-corresponding author Qian-fei Wang, PhD, Beijing Institute of Genomics, Chinese Academy of Sciences in Beijing, China. The sick sister had a particularly acute and aggressive form of the acute myeloid leukemia (AML) known as MLL, or multi-lineage leukemia.
Acute and aggressive leukemia like MLL develops and progresses rapidly in patients, requiring prompt treatment with chemotherapy, radiation or bone marrow transplant. These treatments can be risky or only partially effective. About 70 percent of people with AML respond initially to standard chemotherapy. Unfortunately, five-year survival rates vary between 15-70 percent, depending on the subtype of AML.
The researchers – including co-corresponding author Tao Cheng, MD, Chinese Academy of Medical Sciences & Peking Union Medical College in Tianjin, China – are searching for improved and more targeted treatment strategies. The authors show in their current study that the onset of aggressive and acute leukemia is fueled by a spiraling cascade of multiple gene mutations and what are called chromosomal translocations – essentially incorrect alignments of DNA and genetic information during cell replication.
In comparing the blood cells of both twin sisters, these researchers identified a chromosomal translocation generated what is known as the MLL-NRIP3 fusion leukemia gene. When they activated the MLL-NRIP3 gene in laboratory mouse models, the animals developed the same type of leukemia, but it took a long period of time for them to do so. Researchers said this suggested that there had to be additional cooperative epigenetic and molecular events in play to induce full-blown leukemia.
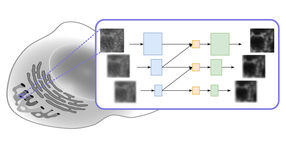
The authors went on to demonstrate that activation of the MLL-NRIP3 fusion leukemia gene cooperated with the molecular cascade (including mutations in SETD2) to cause the multi-lineage form of acute myeloid leukemia (AML). The scientists' initial clue came by looking for additional genomic alterations in the leukemic blood cells of the sick twin sister. They discovered activation of the MLL-NRIP3 fusion leukemia started the molecular cascade that led to bi-allelic (two mutations) in the gene SETD2 – a tumor suppressor and enzyme that regulates a specific histone modification protein called H3K36me3.
During a process called transcriptional elongation, SETD2 and H3K36me3 normally mark the zone for accurate gene transcription along the DNA. In the case of the sick twin sister, the gene mutations and molecular cascade disrupted the H3K36me3 mark, leading to abnormal transcription and the multi-lineage form of acute leukemia.
Researchers then analyzed blood samples from 241 people who had different forms acute leukemia. SETD2 mutations were found in samples from 6.2 percent of those patients. Patients with SETD2 mutations also had a leukemia associated with major chromosomal translocations and disruption of the H3K36me3 mark.
In follow up tests on cell cultures of pre-leukemic cells and mouse models, researchers saw the same progression of gene mutations and related molecular events fuel the growth of leukemic cells. Researchers also noticed mutation of SETD2 activated two genes (MTOR and JAK-STAT) that known contributors to cancer and leukemia. The scientists decided to test two existing targeted molecular inhibitors of MTOR on pre-leukemic cells that are generated by SETD2 gene mutations.
That treatment resulted in a marked decrease in cell growth, indicating that SETD2 mutations activate numerous molecular pathways to generate leukemia. Huang said the tests also demonstrate that there are multiple opportunities to find new molecular targets for developing more effective drugs – in particular those that would target the MLL fusion-SETD2-H3K36me3 pathway for treating acute and aggressive multi-lineage leukemia.
Researchers are following up their current study by identifying additional pathways activated by mutations of SETD2. They also are looking possible new molecular targets and therapeutic strategies for block disruptions in the MLL fusions-SETD2-H3K36me3 pathway.