Signal found to enhance survival of new brain cells
Implications for treating neurodegenerative disease, mental illness
A specialized type of brain cell that tamps down stem cell activity ironically, perhaps, encourages the survival of the stem cells’ progeny, Johns Hopkins researchers report. Understanding how these new brain cells “decide” whether to live or die and how to behave is of special interest because changes in their activity are linked to neurodegenerative diseases such as Alzheimer’s, mental illness and aging.
“We’ve identified a critical mechanism for keeping newborn neurons, or new brain cells, alive,” says Hongjun Song, Ph.D., professor of neurology and director of Johns Hopkins Medicine’s Institute for Cell Engineering’s Stem Cell Program. “Not only can this help us understand the underlying causes of some diseases, it may also be a step toward overcoming barriers to therapeutic cell transplantation.”
Working with a group led by Guo-li Ming, M.D., Ph.D., a professor of neurology in the Institute for Cell Engineering, and other collaborators, Song’s research team firstreportedlast year that brain cells known as parvalbumin-expressing interneurons instruct nearby stem cells not to divide by releasing a chemical signal called GABA.
In their new study, as reported Nov. 10 online in Nature Neuroscience, Song and Ming wanted to find out how GABA from surrounding neurons affects the newborn neurons that stem cells produce. Many of these newborn neurons naturally die soon after their “birth,” Song says; if they do survive, the new cells migrate to a permanent home in the brain and forge connections called synapses with other cells.
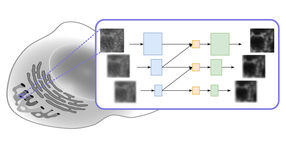
To learn whether GABA is a factor in the newborn neurons’ survival and behavior, the research team tagged newborn neurons from mouse brains with a fluorescent protein, then watched their response to GABA. “We didn’t expect these immature neurons to form synapses, so we were surprised to see that they had built synapses from surrounding interneurons and that GABA was getting to them that way,” Song says. In the earlier study, the team had found that GABA was getting to the synapse-less stem cells by a less direct route, drifting across the spaces between cells.
To confirm the finding, the team engineered the interneurons to be either stimulated or suppressed by light. When stimulated, the cells would indeed activate nearby newborn neurons, the researchers found. They next tried the light-stimulation trick in live mice, and found that when the specialized interneurons were stimulated and gave off more GABA, the mice’s newborn neurons survived in greater numbers than otherwise. This was in contrast to the response of the stem cells, which go dormant when they detect GABA.
“This appears to be a very efficient system for tuning the brain’s response to its environment,” says Song. “When you have a high level of brain activity, you need more newborn neurons, and when you don’t have high activity, you don’t need newborn neurons, but you need to prepare yourself by keeping the stem cells active. It’s all regulated by the same signal.”
Song notes that parvalbumin-expressing interneurons have been found by others to behave abnormally in neurodegenerative diseases such as Alzheimer’s and mental illnesses such as schizophrenia. “Now we want to see what the role of these interneurons is in the newborn neurons’ next steps: migrating to the right place and integrating into the existing circuitry,” he says. “That may be the key to their role in disease.” The team is also interested in investigating whether the GABA mechanism can be used to help keep transplanted cells alive without affecting other brain processes as a side effect.