Drug combination therapy causes cancer cells to 'eat themselves'
Results from a recent preclinical study have shown that a new drug combination therapy being developed at Virginia Commonwealth University Massey cancer Center effectively killed colon, liver, lung, kidney, breast and brain cancer cells while having little effect on noncancerous cells. The results lay the foundation for researchers to plan a future phase 1 clinical trial to test the safety of the therapy in a small group of patients.
"It is still too premature to estimate when a clinical trial will open to further test this drug combination therapy, but we are now in the planning phase and encouraged by the results of these laboratory experiments," says Andrew Poklepovic, M.D., oncologist and member of the Developmental Therapeutics research program at VCU Massey Cancer Center and assistant professor in the Division of Hematology, Oncology and Palliative Care at VCU School of Medicine. "We are also encouraged by the fact that the drugs used in this therapy are either already approved by the FDA to treat certain cancers or are currently being investigated in other clinical trials."
Featured in the journal Molecular Pharmacology, the study led by Paul Dent, Ph.D., demonstrated that the drugs sorafenib and regorafenib synergize with a class of drugs known as PI3K/AKT inhibitors to kill a variety of cancers. Sorafenib and regorafenib work by blocking the production of enzymes called kinases, which are vital to the growth and survival of cancer cells. Sorafenib is currently approved by the FDA to treat kidney and liver cancers, and regorafenib is currently approved for the treatment of colorectal cancer. However, sorafenib and regorafenib do not directly affect PI3K and AKT kinases, which are also very active in promoting cancer cell survival. The addition of a PI3K/AKT inhibitor to the combination of sorafenib and regorafenib dramatically increased cell death and was even effective against cells with certain mutations that make one or the other drug less effective.
"We know that there are certain cellular processes that are frequently dysregulated in cancers and important to cell proliferation and survival, but if you shut down one, then cells can often compensate by relying on another," says Dent, Universal Corporation Distinguished Professor for Cancer Cell Signaling and member of the Developmental Therapeutics research program at VCU Massey Cancer Center as well as vice chair of the Department of Neurosurgery at VCU School of Medicine. "We are blocking several of these survival pathways, and the cancer cells are literally digesting themselves in an effort to stay alive."
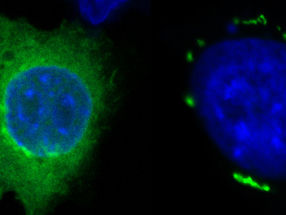
Results of the study showed that the combination therapy killed the cells by physically interacting with molecules to block the survival pathways and induce a toxic effect known as autophagy. Autophagy is a protective process where cells metabolize themselves when starved of the resources needed to survive.
"Many groups are trying the approach of inhibiting two survival signaling pathways, but our approach takes this further by blocking significantly more of these pathways," says Dent. "Our findings could benefit many different cancer patients based on the broad range of effects seen in multiple cancer types."
Most read news
Topics
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.