Nanotechnology helps track and improve drug action in pancreatic cancer
Advertisement
UK and Australian scientists have been able to show ways in which we can markedly improve drug targeting of solid tumours, using tiny 'biosensors' along with new advanced imaging techniques.
In real time and in three dimensions, these technologies can show us how cancers spread and how active cancer cells respond to a particular drug. They can also tell us how much, how often and how long to administer drugs. Finally, using preclinical models of the disease, they can guide the use of 'combination therapies', techniques that enhance drug delivery by breaking up the tissue surrounding a tumour.
The study was performed by Dr Paul Timpson of the Garvan Institute of Medical Research and Professor Kurt Anderson of the Beatson Institute for Cancer Research in Glasgow, UK. PhD student Max Nobis studied the signaling protein 'Src', which becomes activated to drive invasive pancreatic cancer, and looked at how it could best be deactivated by a small molecule inhibitor — currently in phase II clinical trials — known as 'dasatinib'. Their findings are published in the journal Cancer Research.
"We have already shown that Src is activated in pancreatic tumours and we knew that dasatinib deactivates Src and could partially reduce the spread of this form of cancer. Through a collaborative partner in the US, we had access to FRET (Fluorescence Resonance Energy Transfer) imaging technology," said Dr Paul Timpson.
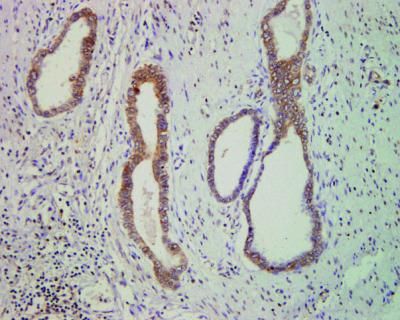
"Until now, we have been limited to studying tumour signalling in two dimensions – and lacked a dynamic way of reporting on drug targeting in live tumour tissue. Nanotechnology opens up a portal into living tissue that allows us to watch cancers spreading, and to determine which parts of a tumour we should be targeting with drugs."
"This imaging technology has allowed us to map areas within the tumour that are highly aggressive, allowing us to pinpoint regions of poor drug delivery deep within a tumour at sub-cellular resolution. We can then see where we need to improve on drug delivery to improve clinical outcome."
It has been hard to treat pancreatic tumours because they are extremely dense with collagen and have poor blood vessel networks for delivering drugs.
Professor Kurt Anderson observed that combination therapies can now be used to break down collagen, weakening tumour architecture and making it easier to get the drugs where they need to be. "The trick is to break down the structure just enough to get the drug in, but not so much that you damage the organ itself," he said.
"These new FRET technologies help us gauge what is just enough and not too much."
"These are very exciting discoveries – we now have spatial and temporal information about cancer behaviour that we've never had before, as well as the nanotechnology to monitor and improve drug delivery in hard to reach tumour regions."