Using new ways to study a devastating disease: Researchers observe Alzheimer's disease in cultures and living tissue
Advertisement
Beta amyloid plaques - the clumps of protein molecules that build up in the brains of people afflicted with Alzheimer's disease - have long been the focus of researchers searching for ways to treat the devastating illness. At Cornell, a group of scientists on the Ithaca and New York City campuses are studying how the plaques' precursor molecules form, what makes them clump together and why the cells normally responsible for trash removal within the brain fail to gobble them up. The work could eventually lead to a way of stimulating brain cells to destroy the precursor molecules, the way the body's white blood cells destroy everyday debris and invaders such as viruses and harmful bacteria.
Fred Maxfield, the Israel Rogosin Professor of Biochemistry and chair of the Department of Biochemistry at Weill Cornell Medical College (WCMC), and Gunnar Gouras, associate professor of neurology and neuroscience at WCMC, lead laboratories in which researchers are developing new ways to study how the plaques affect nerve cells (neurons). Now, in partnership with Watt Webb, professor of applied physics and the S.B. Eckert Professor in Engineering in Ithaca, Maxfield and Gouras hope to go further - to study the plaques in living tissue and to test if they can be destroyed by microglial cells, the brain's equivalent to the body's macrophages (the white cells that attack invaders).
Beta amyloid plaques are actually strings of protein molecules, called A beta, which are manufactured inside neurons and then are released outside the cells. In patients with Alzheimer's, they accumulate and damage neurons in ways that are not well understood.
"We're interested in why microglial cells don't degrade amyloid and whether they might degrade it in some circumstances," said Maxfield.
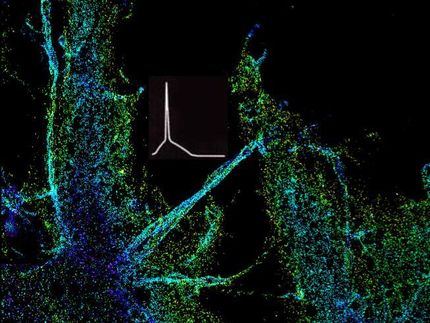
Using multiphoton microscopy (MPM), a technique developed in Webb's laboratory, the WCMC researchers hope to find the answer. MPM works by focusing an intense, high-precision laser beam on a sample, using the combined energy of two photons to trigger targeted molecules to emit fluorescent light.
"We discovered that the amyloid plaques are intrinsically fluorescent," said Webb. That property, and the fact that the technique is not destructive to tissue, will allow researchers to use MPM to see beta amyloid in the brains of living mice genetically engineered to develop an Alzheimer's-like disease.
One key to prompting the brain's own defenses against the disease may have to do with the pH of the digestive organelles in microglia. If they can be made more acidic, Maxfield says, they may start to digest the amyloid molecules on their own. That hypothesis has been tested with promising results in cultured cells in the laboratory, but the technique needs further study in living systems.
"Sometimes you find out that things don't behave the same in the animal as in cell culture," said Maxfield. "It's important to find that out as soon as possible."