"Sticky" mice lead to discovery of new cause of neurodegenerative disease
Advertisement
When a faulty protein wreaks havoc in cells and causes disease, researchers are usually quick to point the finger at a wayward gene. Now scientists are learning that some neurodegenerative diseases can develop even though a gene is perfectly normal. The diseases can be caused when the genetic instructions contained in the gene are not executed properly, leading to a lethal buildup of malformed proteins in brain cells.
The new studies by Howard Hughes Medical Institute (HHMI) investigator Susan L. Ackerman and colleagues at The Jackson Laboratory point to a novel mechanism behind the buildup of the toxic sludge that accumulates in neurons. Researchers have long known that neurodegenerative disorders can be caused by the gradual yet persistent accumulation of misfolded proteins in neurons that eventually triggers cell death. But this new mechanism points to errors in executing the genetic instructions, which are distinct from known causes of neurodegenerative diseases, such as Alzheimer's and Huntington's diseases. Susan L. Ackerman and her colleagues reported their findings in Nature. Ackerman's group collaborated on the studies with co-author, Paul Schimmel at The Scripps Research Institute.
The researchers made their discovery by studying mice with a mutation called sticky (sti). Although named for the sticky appearance of their fur, the mice harbor much more serious problems beneath their unkempt coats: poor muscle control, or ataxia, due to death of Purkinje cells in a region of the brain called the cerebellum.
No one knew why Purkinje cells were dying in sticky mutant mice. To find out, Ackerman and her colleagues searched for the gene that was disrupted by the sti mutation. They were surprised to find a subtle defect in a gene that codes for part of the cell's protein synthesis machinery -- an enzyme called alanyl tRNA synthetase. This enzyme is responsible for loading, or "charging" the amino acid alanine onto transfer RNAs (tRNAs). Transfer RNAs transport individual amino acids to the cell's protein synthesis machinery, where they are added to the growing stringlike protein molecules being manufactured there. Each tRNA is designed to carry only one of the 20 amino acids used to build proteins, and accurate loading is critical for the resulting protein to have the correct structure.
Ackerman said that when the team began its studies, it did not expect that such a fundamental defect in protein synthesis could be behind the neurodegeneration they had observed in sticky mice. "There were a lot of candidate genes in the chromosomal region containing the sti mutation," she said, "and this gene was actually the last candidate gene we investigated. It seemed to us that a mutation in a gene so fundamentally important for protein translation would cause early lethality. But when we couldn't find a defect in any of the other genes in the sti region, we decided to look closer at the tRNA synthetase gene. And there it was."
To set aside any doubts they might have had about the role of the tRNA synthetase gene, Ackerman and her colleagues showed that they could correct the pathology in the sticky mouse mutants by using genetic techniques to insert a normal version of the tRNA synthetase gene.
To understand the specific defect in the tRNA synthetase gene, Ackerman and her colleagues collaborated with Schimmel, whose research has concentrated on the biochemistry of synthetases. Molecular studies by Schimmel and his colleagues revealed that the defect in the sti mutant mouse occurred in a region of the synthetase enzyme that "edits" the loading of the correct amino acid, alanine, onto its carrier tRNA. This editing enables the enzyme to reject incorrect amino acids.
The researchers found that the mutant enzyme would charge an incorrect amino acid, serine, which resembles alanine, to tRNAs meant to carry only alanine. That meant that these tRNAs, said to be mischarged, would incorporate the incorrect amino acid into proteins. Although proteins begin as long strings of amino acids, they are ultimately folded into intricate three-dimensional shapes in order to function properly. Malformed proteins resulting from serine substitution could fold improperly, clogging and eventually killing cells.
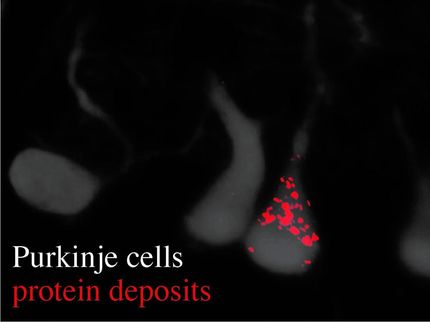
When Ackerman and her colleagues examined the Purkinje cells of sticky mouse mutants, this is exactly what they saw. They also detected biochemical evidence that the cells were making an unsuccessful effort to tag and destroy the accumulating misfolded proteins.
"Our finding that this mechanism underlies a neurodegenerative disease was highly unexpected," said Ackerman. "It was perfectly obvious that mischarged tRNAs, may generate misfolded proteins. But what surprised us was that such a small increase in mischarged tRNAs could have such a devastating result in terms of neuronal survival. Nobody I know of has put forth such a mechanism for human neurological disease."
Ackerman speculates that human disease could arise when a mild inherited defect in a tRNA synthetase led to a subtle increase in malformed proteins, which could cause the death of particularly vulnerable cells such as Purkinje cells. "This mouse model shows that such a mechanism is possible," she said. "The sticky mouse has a mild editing defect that still allows it to produce offspring.
"So, a major question to be explored in human populations is whether the subtle loss of translational fidelity from such a defect could lead to various human diseases - particularly those that involve the accumulation of misfolded proteins," she said.
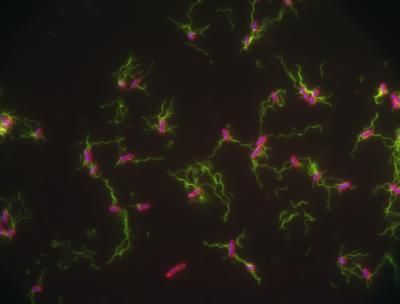
Ackerman and her colleagues are conducting further studies to understand why Purkinje cells are particularly vulnerable to defects in protein synthesis. They are also exploring how the actions of other genes in the cell can alleviate the pathology caused by protein misfolding.