New Data Suggest Vertex's Oral Hepatitis C Virus Protease Inhibitor VX-950 May Reduce Liver Injury
New data show that patients with genotype 1 hepatitis C virus (HCV) infection treated with VX-950, an investigational oral HCV protease inhibitor being developed by Vertex Pharmaceuticals Incorporated, rapidly achieved substantial reductions in alanine aminotransferase (ALT) levels after 14 days of treatment.
Data from a 14-day clinical study demonstrated that treatment with any one of three doses of VX-950 resulted in median serum ALT declines of 25-32 U/L in all dose groups. In the placebo group, a median 8 U/L increase was observed. Prior to treatment with VX-950, serum ALT levels were elevated in approximately 70 percent of patients in the study. In the VX-950 dose groups, 83 percent (15 of 18) of patients with elevated ALT levels at baseline (prior to treatment) had achieved normalization of ALT levels at day 14, compared to 0 percent (0 of 6) in the placebo group. Elevated ALT levels are common in HCV patients and are considered to be a marker of liver injury due to HCV infection. Mean levels of serum neopterin also were observed to decrease with VX-950 treatment in the study. Decreased neopterin levels may be a further signal of a reduction in inflammation associated with HCV infection.
A study of viral isolates from patients at baseline in a 14-day clinical study found heterogeneity among viral sequences in the HCV protease domain. In vitro analysis indicated that all baseline viral isolates were sensitive to VX-950.
"To date, data from early clinical studies have suggested that VX-950 is well-tolerated and can rapidly reduce HCV viral levels in patients over a short treatment period," said John Alam, M.D., Senior Vice President of Drug Evaluation and Approval at Vertex. "In addition, we now have evidence that treatment with VX-950 appeared to lead to a dramatic decline in markers of liver injury associated with viral infection."
Other news from the department research and development

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
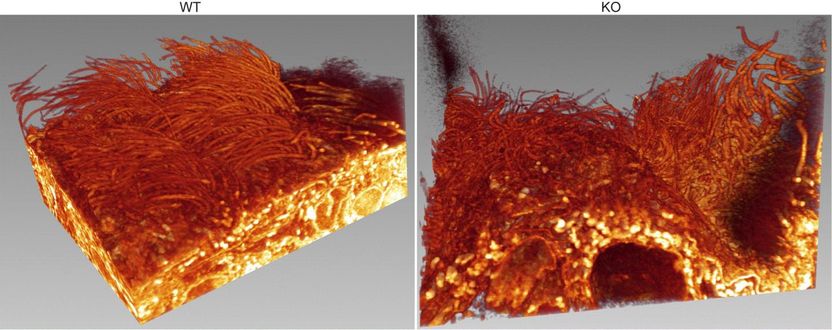
Loss of essential protein in the choroid plexus epithelium linked to hydrocephalus
Eurofins Medigenomix offers fast DNA sequencing service - Roche Diagnostics` Genome Sequencer System Powers Eurofins | Medigenomix / MWG Biotech
Cambridge Major To Partner with Novacta Biosystems
Spinal cord neurons that control pain and itch

Biovertis Information-driven drug design AG - Wien, Austria