UF researchers hope clinical trial will lead to new sepsis treatment
University of Florida researchers are part of a nationwide clinical trial to evaluate whether an anti-cancer medication can be effective against sepsis and septic shock.
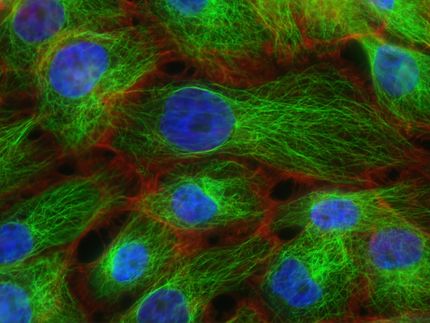
Sepsis is thought to blunt the immune system in ways similar to some kinds of cancer through PD-1, a protein emitted by certain cells in the body. Nivolumab, an immunotherapy drug approved by the Food and Drug Administration to treat patients with certain types of non-small cell lung cancer and other types of the disease, blocks PD-1 in cancer patients and helps the immune system recognize and destroy diseased tissue.
The clinical trial seeks to determine whether blocking PD-1 can also boost the immune system in patients with severe sepsis or septic shock. UF is the only center in Florida, and one of four in the Southeast, recruiting participants.
“Think of your immune system as a crackling fire, burning at a steady pace. Sepsis is like throwing gasoline on that fire. You get a huge flare and explosion but afterward, you are left with smoldering coals that do not work. The point is to get those smoldering coals back to a crackling fire again,” said UF’s lead investigator, Scott C. Brakenridge, M.D., MSCS, FACS, an assistant professor of surgery and anesthesiology in the UF College of Medicine’s division of acute care surgery.
Sepsis is an illness or complication in which the body has a severe, overwhelming response to infection. That response can induce tissue damage, organ failure and death. What differentiates sepsis from infection is the significant host response to an infectious virus, bacteria, fungus or parasites.
“Instead of trying to blunt that immune explosion, we are focusing on ways to get the immune system back on its feet after it’s been knocked down,” Brakenridge said. “The goal is to prevent prolonged immunosuppression so the body can fight infectious challenges.”
Sepsis is the most expensive condition treated in U.S. hospitals, with annual costs exceeding $20 billion, according to the Agency for Healthcare Research and Quality.
“The early care of sepsis has improved dramatically, and in-hospital mortality has decreased substantially. The majority of sepsis survivors progress into chronic critical illness characterized by prolonged stays on intensive care units, cognitive and functional disabilities, sepsis relapse, discharge to long-term health care or rehabilitation facilities, and death,” said Frederick A. Moore, M.D., FACS, MCCM, the program director of the UF Sepsis and Critical Illness Research Center and a professor and chief in the division of acute care surgery in the UF College of Medicine.
Specifically, UF Health clinical and basic science researchers recognized a new predominant type of chronic critical illness that is occurring with an increased frequency in surgical ICUs — persistent inflammation, immunosuppression and catabolism syndrome — for which there are no effective interventions and clinical outcomes are poor.
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.