Artificial bile ducts grown in lab could help treat liver disease
Cambridge scientists have developed a new method for growing and transplanting artificial bile ducts that could in future be used to help treat liver disease in children, reducing the need for liver transplantation.
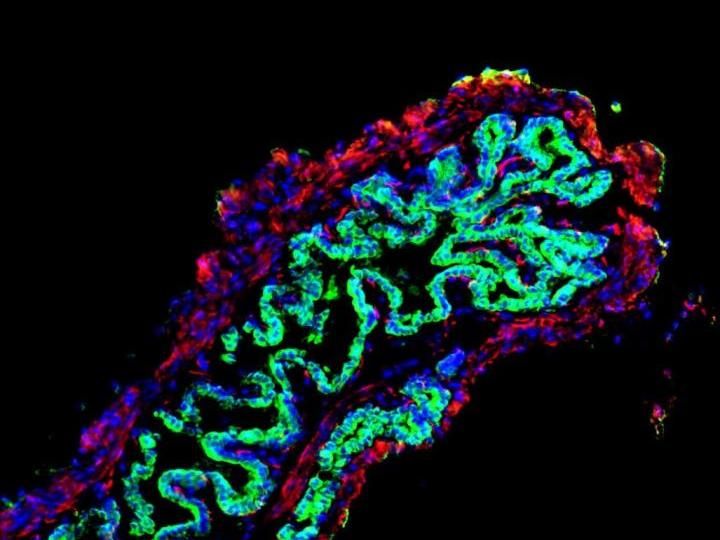
This is an image of a mouse gallbladder following repair with a bioengineered patch of tissue incorporating human 'bile duct' cells, shown in green. The human bile duct cells have fully repaired and replaced the damaged mouse epithelium.
Fotis Sampaziotis
The researchers grew 3D cellular structure which, once transplanted into mice, developed into normal, functioning bile ducts.
Bile ducts are long, tube-like structures that carry bile, which is secreted by the liver andis essential for helping us digest food. If the ducts do not work correctly, for example in the childhood disease biliary atresia, this can lead to damaging build of bile in the liver.
The study suggests that it will be feasible to generate and transplant artificial human bile ducts using a combination of cell transplantation and tissue engineering technology. This approach provides hope for the future treatment of diseases of the bile duct; at present, the only option is a liver transplant.
The University of Cambridge research team, led by Professor Ludovic Vallier and Dr Fotios Sampaziotis from the Wellcome-MRC Cambridge Stem Cell Institute and Dr Kourosh Saeb-Parsy from the Department of Surgery, extracted healthy cells (cholangiocytes) from bile ducts and grew these into functioning 3D duct structures known as biliary organoids. When transplanted into mice, the biliary organoids assembled into intricate tubular structures, resembling bile ducts.
The researchers, in collaboration with Mr Alex Justin and Dr Athina Markaki from the Department of Engineering, then investigated whether the biliary organoids could be grown on a 'biodegradable collagen scaffold', which could be shaped into a tube and used to repair damaged bile ducts in the body. After four weeks, the cells had fully covered the miniature scaffolding resulting in artificial tubes which exhibited key features of a normal, functioning bile duct. These artificial ducts were then used to replace damaged bile ducts in mice. The artificial duct transplants were successful, with the animals surviving without further complications.
"Our work has the potential to transform the treatment of bile duct disorders," explains Professor Vallier. "At the moment, our only option is liver transplantation, so we are limited by the availability of healthy organs for transplantation. In future, we believe it will be possible to generate large quantities of bioengineered tissue that could replace diseased bile ducts and provide a powerful new therapeutic option without this reliance on organ transplants."
"This demonstrates the power of tissue engineering and regenerative medicine," adds Dr Sampaziotis. "These artificial bile ducts will not only be useful for transplanting, but could also be used to model other diseases of the bile duct and potentially develop and test new drug treatments."
Original publication
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
CRISPR/Cas9 Silences Gene Associated with High Cholesterol
Genetic causes of canine mammary tumors
Evolva reaches milestone in BASF collaboration
MedGenome secures series C funding

Evotec initiates ground-breaking for new biologics facility J.POD® Toulouse - The manufacturing facility is expected to be operational in H2 2024 and will create upwards of 150 new high-skill jobs

Fujifilm Invests $188 Million in New Cell Culture Media Manufacturing Facility - The new facility is planned to ensure that FUJIFILM Irvine Scientific can meet increasing market demands