Evolution of ebola virus resulted in increased human infectivity
Scientists have studied the evolution of the Ebola virus during the recent West African outbreak to determine how unprecedented numbers of humans became infected.

Evolution of ebola virus resulted in increased human infectivity
BBSRC
An international study led by Professor Jonathan Ball at The University of Nottingham, has shown that genetic changes which took place as the virus was transmitted from human to human increased infectivity during the epidemic.
Professor Ball, Professor of Molecular Virology in the University’s School of Life Sciences, said: “Whether or not the virus genetic changes that arose during the outbreak were affecting the virus’s ability to infect humans was a moot point, but I was fairly sure it must be happening – never before had this virus had such an opportunity to fine tune its ability for human transmission.”
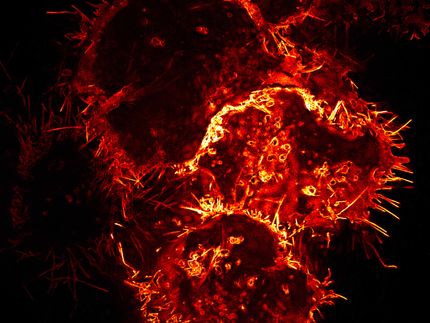
To test their theory the researchers focussed on the surface protein, which the virus uses to bind to a protein receptor on the surface of the target cell in order to gain entry. It was then a case of identifying the genetic changes that accumulated in the surface protein during the outbreak, generating synthetic clones of these, then seeing if these mutant proteins behaved differently to that seen in viruses sampled at the start of the outbreak.
Commenting on the approach the researchers had to take, Dr Richard Urbanowicz, a research fellow in the School of Life Sciences, said “Working with ebolavirus isn’t very easy – you need access to special high containment labs to handle the whole virus – and not many places have these. So instead we generated particles of a modified mouse virus related to HIV that had been tricked into coating itself with the ebolavirus surface protein. These pseudoviruses, as they are known, would then mimic how ebolavirus gained entry into a cell, but importantly once inside the cell they would not replicate”. This meant the studies could be performed without the need for ultra-high containment facilities.
When the scientists infected human liver cells grown in a test tube with these pseudoviruses the data was clear – a number of genetic changes that occurred during the outbreak increased infectivity.
“When I saw the first set of data the trend was so clear you didn’t really need to do any stats to see the effect the changes were having – without doubt many of the genetic changes were increasing infectivity in human cells,” Dr Urbanowicz said . The effects were not restricted to liver cells – similar trends were also seen for human cells derived from lung.
One change in particular, a substitution of an amino acid that is involved in receptor binding, was particularly striking: not simply because it dramatically increased infectivity, but also because it was present in viruses that dominated the West African outbreak.
The studies threw up one more twist. Mutations that increased infectivity in human cells seemed to reduce the ability of the protein to mediate entry into cells obtained from fruit bat cells, which are thought to be the natural host for ebolavirus.
The unprecedented number of human to human transmissions that occurred during the recent ebolavirus outbreak gave the virus an opportunity to become adapted to humans and the study’s data suggests that this was an opportunity the virus didn’t miss.
It’s not known for sure whether these changes affected the virus’s ability to transmit during the outbreak or were associated with more severe disease – further studies will be needed to try to determine that – but Prof Ball does think that the study has wider implications: “I think our study reminds us that if you take a virus and allow it to infect a new host for a considerable amount of time, eventually it may acquire a set of mutations that will benefit it, either increasing its ability to spread or changing the disease that it causes. In order to be prepared we need to know whether similar things are occurring in other outbreaks such as the ongoing Zika and MERS-coronavirus epidemics.”