New model developed to study inflammatory bowel disease in human biopsy samples
Inflammatory bowel disease (IBD) is a complex condition that requires a lifetime of care and increases a person's cancer risk. But its origins are still a mystery. Now, a team of researchers have created a new culture model of the human intestine where living tissue from a patient biopsy can be preserved and studied for days.
The model will enable researchers to study potential disease causes and test new drugs to treat IBD, said study author Amy Dawson, a postdoctoral researcher in the lab of John Greenman at the University of Hull, U.K. The study was performed in collaboration with Morten Jacobsen at the University of Oslo in Norway, the senior lead on the study.
"The new model enables studies of the complex interactions between host cells, mucus production, and gut microbes in a system that closely mimics the situation in human patients," Dawson said.
Although localized inflammation and differences in the gut microbiome have been linked to the symptoms of ulcerative colitis and Crohn's disease - the two forms of IBD - the precise cause of these disorders is still unknown. Studies of IBD are typically performed using cell culture experiments or animal models, which don't mimic the precise conditions that occur in the gut of human patients. When using biopsied tissue, researchers rely on a device known as the Ussing chamber, which clamps the sample in place under static growth conditions - crushing parts of the sample and keeping it viable for approximately eight hours. Instead of such static culture conditions, Dawson and her colleagues turned to a dual flow microfluidic chamber - which removes wastes and supplies nutrients via continuous liquid streams - and can keep tissues viable for prolonged periods of time.
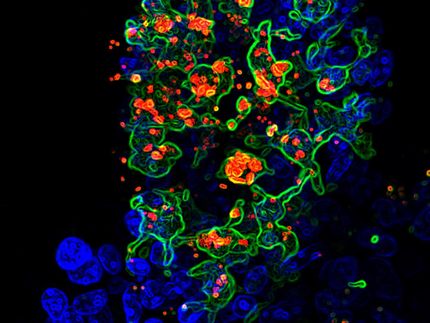
To study biopsied intestinal samples, the research team engineered a microfluidic chamber where intact tissues can be inserted in a known orientation. Fluid flow on either side of the tissue mimicked the luminal and serosal surfaces of the gut within the body. Tissue samples were collected from patients who were undergoing biopsies after a diagnosis of IBD, and from patients suffering colon cancer whose tissues were unaffected by IBD-linked changes.
In the first 24 hours, tissues released large amounts of lactate dehydrogenase, an enzyme marker linked to cell death - likely because cells were damaged during the surgery and setting up the device, Dawson explained. But after this initial spike, enzyme functions and microscopic analysis showed that the tissues remained alive and viable for up to 72 hours within the dual-flow device.
"You would expect some form of decay after removal from the human body," Dawson said. "But the tissue remains functional for a significant amount of time."
Nearly 85 percent of patient samples could be successfully used to create such IBD models. Using these biopsies to test different treatment plans could also help to quickly identify personalized plans to treat patients' disorders.
"The model is relatively easy to establish in any laboratory and can be applied to many kinds of tests, as it is more similar to the reality of the human body," Dawson added.
In future studies, the team plans to use the model to better understand how microbes, host factors and inflammatory markers interact to produce the hallmarks of inflammatory disease in the intestine.
"It's crucial to understand the gut bacteria and this interplay," said Dawson. "At the moment, there are no consistent patterns amongst people who have IBD and those who don't."
Original publication
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Capsule_(pharmacy)
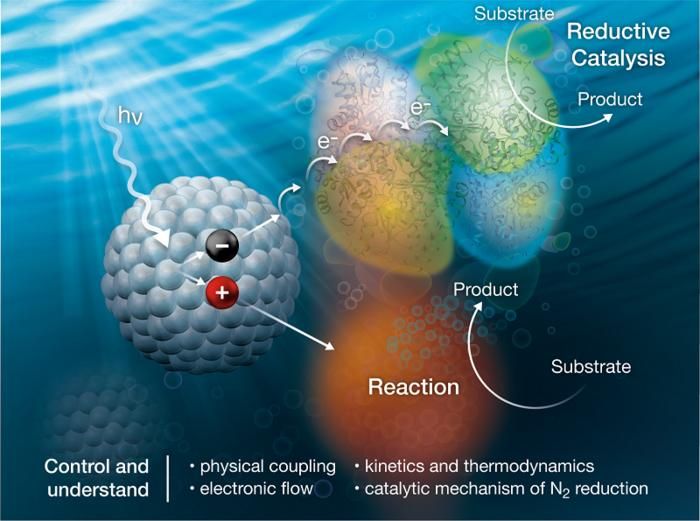
Powering enzymes with light to make ammonia - Scientists examine how molecular systems made of nanocrystals and proteins support the production of ammonia using light.
Overactive enzyme causes hereditary hypertension - Hope for new and more effective therapeutic approaches for hypertension

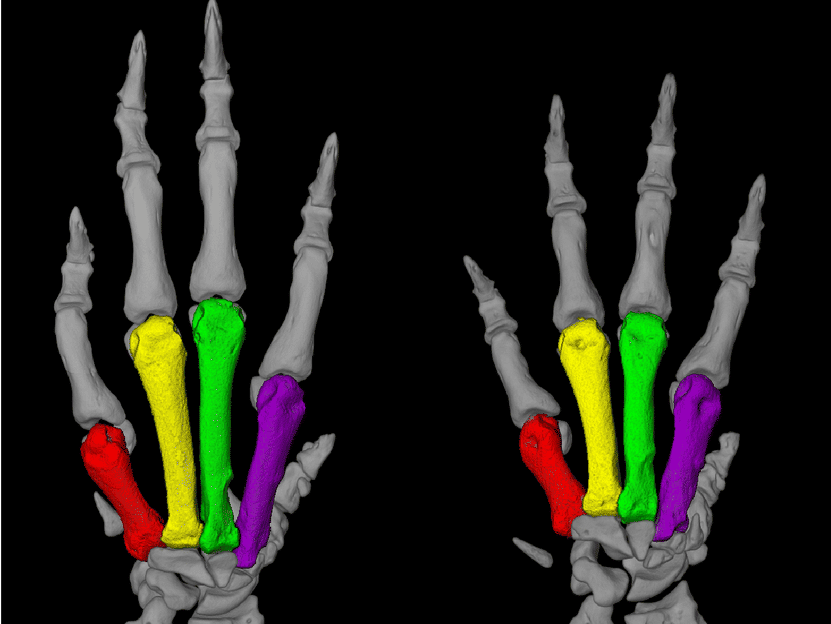
So-called junk DNA plays critical role in mammalian development - Knocking out transposon promoter leads to pup death in mice; similar promoters found in many mammals
Medicinal_chemistry
Glucagon_rescue
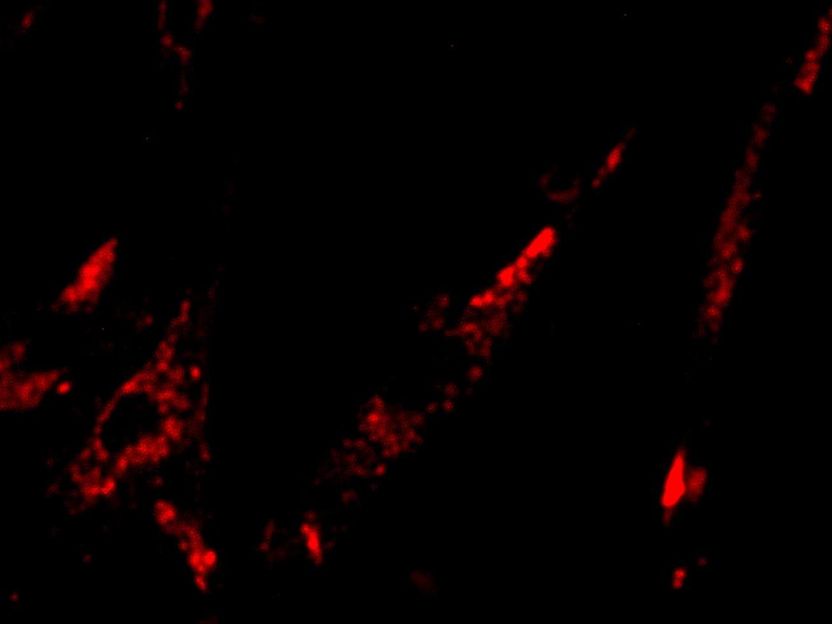
Toward glow-in-the-dark tumors - New fluorescent probe could light up cancer
Devil_facial_tumour_disease