New insights into latent HIV infections
In spite of ever more effective therapies, HIV keeps managing to survive in the body. A comprehensive project conducted by the Austrian Science Fund FWF has clarified the molecular processes which contribute to this effect. In the process, approaches were discovered for possible therapies to combat the hidden reservoir formed by the virus.
Thanks to modern therapies, HIV infections have become controllable – but these treatments cannot provide a cure. Antiretroviral therapies do indeed manage to keep the number of HI-virus particles in the blood of those infected so low that the outbreak of AIDS is prevented. But the virus cannot be removed entirely. Because it is a master at hiding.
Cellular Hiding Place
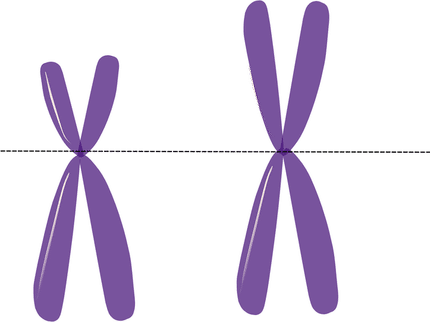
One hiding place of the virus that is known are special immune cells called macrophages. The virus can survive inside these cells – beyond the reach of drugs. A team led by Regina Grillari from the Department for Biotechnology at the University of Natural Resources and Life Sciences, Vienna, has found out how the virus can also manipulate the cells to make them more stress-resistant and longer-living. The main focus of the project lay on the enzyme, telomerase, which is active when cells divide and prevents chromosome shortening. Little has been known until now about its activity in cells which, like macrophages, do not divide. The results presented by Grillari were all the more astonishing, as she explains. “We were able to show that the HIV virus induces telomerase activity in macrophages. This was surprising to the extent that the enzyme’s known function was connected to cell division which in this case doesn’t even take place.”
No Function?
A further result showed that telomerase in macrophages does not even pursue its real function – that of lengthening chromosomes – in spite of activation by the HI-virus. Another experiment then supplied clear indications of the role played in this case by telomerase in infected cells. To do so, the reactions of infected and non-infected macrophages to so-called oxidative stress were investigated; oxidative stress is also increased by HIV infections. Results showed that infected cells are able to cope with this stress much better than non-infected ones – and that this is connected to telomerase activation.
As Grillari explains: “It seems that the hidden virus particles make their host cells more stress-resistant through telomerase activation, thereby securing their own survival in the long term. A sensible strategy from the perspective of the virus.”
“Elite” Research
In another part of the project, so-called “elite” patients were examined. Although these patients are infected with HIV, their bodies manage to so heavily restrict replication of the virus that they can live free of symptoms for years with no therapy. While it is not known how this happens, there are indications that special RNAs (miRNAs) play a role here. Grillari and her team analyzed whether there were differences in the types and frequency of miRNAs circulating in the blood between infected elite patients, “normally” infected and healthy persons. Three different types were indeed identified which occurred in markedly different concentration in the plasma of “elite” patients than in the other groups. Grillari comments: “In future we could use them as biomarkers in order to determine whether people infected are in the ‘elite’ category or not, and thereby to tailor a therapy to their particular status.” The study also succeeded in showing that two of the miRNAs restrict the replication of the virus under laboratory conditions – which means that they could certainly be interesting for new therapeutic approaches.
Altogether in this FWF project, Grillari’s team succeeded in identifying molecular mechanisms which the HI-virus uses to make macrophages more resistant, thus reprogramming them to become an ideal virus reservoir. At the same time, starting points were found from which it may be possible to combat this reservoir formation with miRNAs.
Most read news
Topics
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Brain-computer interface, developed at Brown, begins new clinical trial

MSD to acquire EyeBio - Start-up developing new treatment options for patients with retinal diseases
Anti-idiotypic

Scientists use novel ink to 3D-print ‘bone’ with living cells - 3D printers may one day become a permanent fixture of the operating theatre
Novel sensor implant radically improves significance of NMR brain scans - Researchers present a new method that shows single neuron data
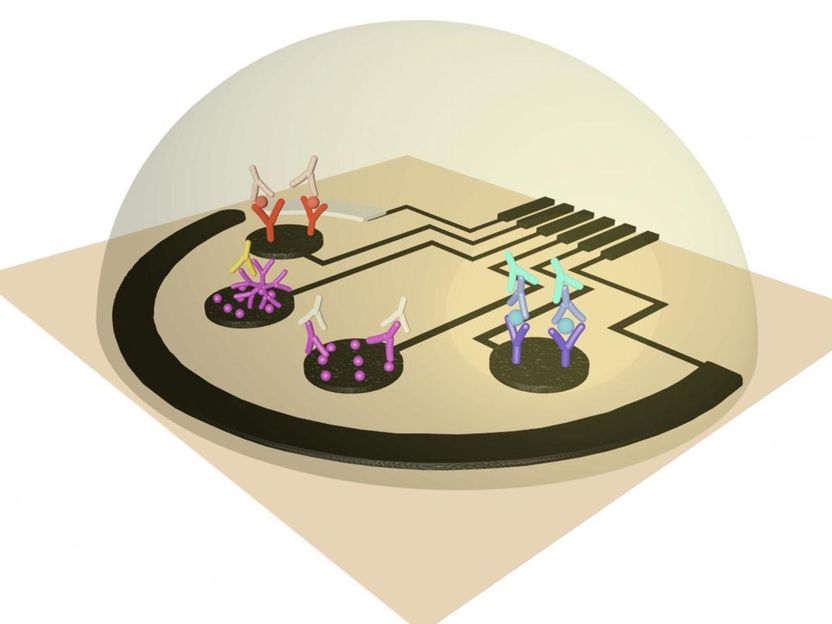
Researcher unveils sensor that rapidly detects COVID-19 infection - New test may enable the at-home diagnosis of a COVID infection through rapid analysis of small volumes of saliva or blood in less than 10 minutes
Evident to accelerate its growth and innovation - Olympus Agree on Transfer of Evident to Bain Capital
Category:Uncategorised_pharmacology_articles
Molecular Devices and Cytena Partner collaborate in single cell printing
Crouzon_syndrome