Purdue researchers discover signaling cascade that drives fatty tumors
A common cell signaling pathway that controls differentiation of stem cells may also control the formation of tumor cells in fat, according to a Purdue University study.
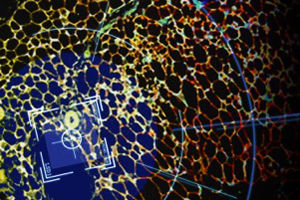
This signaling pathway, called Notch signaling, has been widely reported to determine the identity and control the differentiation of a variety of stem cells in different tissues. Notch signaling occurs between two neighboring cells, in which one cell sends a signal to the neighbor cell to control its gene transcription program that determines the identity of the neighbor cell.
Stem cells are basically blank slates, waiting to become a particular, differentiated type of cell. In fat cells, that differentiation is controlled by a regular pattern of Notch signaling. Aberrant suppression or activation of Notch signaling may disrupt the normal differentiation process and maintenance of stem cells.
Shihuan Kuang, professor of animal sciences at Purdue, had earlier determined that when Notch signaling is suppressed, white fat cells, which are linked to obesity due to their ability to accumulate excessive lipids, turn into beige fat cells. Beige fat is more metabolically active and breaks down lipids by turning them into heat.
It's possible that humans evolved to build up white fat, which acted as insulation but also as an energy store and endocrine organ. The physical activity required to live off the land would have kept white fat from over accumulating in most people. As we have become less active, however, energy stored in white fat is not spent and its over-accumulation is associated with metabolic diseases such as diabetes, obesity and some types of cancer.
"Beige fat, if you consider human physiology, is wasting energy," said Pengpeng Bi, a former Purdue postdoctoral fellow and lead author. "But it would be good for us now because we are overfed and more inactive."
A previous study published by Bi and Kuang in Nature Medicine has shown that when Notch signaling is inhibited in the fat cells of mice, the animals are obesity-resistant and less likely to develop diabetes when fed a high-fat diet.
This time, the group wanted to know what would happen if Notch signaling is overactive in fat cells. The findings, published in the Journal of Experimental Medicine, show that when Notch signaling is turned up beyond normal levels in mice, those same white fat cells degenerate and turn cancerous.
"A normal amplitude of Notch signaling is required for a human or animal to develop, but overactive Notch signaling is linked to cancer in several cell types," Kuang said. "Our study demonstrates for the first time that Notch activation is sufficient to drive the development of malignant tumors in fat tissue, termed liposarcoma."
Tumors of this kind aren't common, but Kuang said that liposarcomas can be devastating and hard to treat, mainly because surgical excision, the standard treatment, often leads to uncontrolled recurrence that causes death. This new study suggests that pharmacological inhibition of Notch signaling may be effective in treating a subtype of liposarcomas in humans.
The degeneration of fat cells when Notch signaling is overactive also makes the transgenic animals created in the current study ideal for modeling another metabolic condition – lipodystrophy. In patients with lipodystrophy, the scarcity of white fat cells forces other organs, including the liver and muscles, to pick up additional body lipids. Even though they are thin, lipodystrophy patients have the hallmark signs of obesity, including high blood sugar, fatty liver and insulin resistance.
Understanding how overactive Notch signaling shrinks fats cells and turns them into cancerous cells is the emphasis of Kuang's future work.
"We hope the study could give clues on the development and treatment of metabolic diseases including obesity, type 2 diabetes, lipodystrophy and liposarcomas," Kuang said.
Original publication
Pengpeng Bi, Feng Yue, Anju Karki, Beatriz Castro, Sara E. Wirbisky, Chao Wang, Abigail Durkes, Bennett D. Elzey, Ourania M. Andrisani, Christopher A. Bidwell, Jennifer L. Freeman, Stephen F. Konieczny, and Shihuan Kuang; "Notch activation drives adipocyte dedifferentiation and tumorigenic transformation in mice"; J Exp Med; 2016