Global trial shows CAR T therapy can lead to durable remissions in non-Hodgkin's lymphoma
Advertisement
In an update to a global clinical trial stretching from Philadelphia to four continents, the chimeric antigen receptor (CAR) T cell therapy Kymriah® (tisagenlecleucel, formerly CTL019) led to long-lasting remissions in patients with relapsed/refractory (r/r) diffuse large B-cell lymphoma (DLBCL). The most recent results from the trial will be presented at the 60th American Society of hematology (ASH) Annual Meeting and Exposition in San Diego. Stephen J. Schuster, MD, director of the Lymphoma Program at the Abramson Cancer Center of the University of Pennsylvania, was the principal investigator on the trial, which is known as JULIET and has already led to approval by the U.S. Food and Drug Administration as well as by the European Commission, Health Canada, and Swissmedic. Another data set from the JULIET trial with an earlier cut-off date will also be published simultaneously.
JULIET included 27 sites in 10 countries across North America, Europe, Australia, and Asia. According to the data presented at ASH, 115 patients with r/r DLBCL received an infusion of CAR T cells. The overall response rate of evaluable patients was 54 percent, with 40 percent achieving a complete response. The median duration of those responses was not reached at a median follow-up of 19 months.
"These findings are consistent with what we've shown in our single-site studies here at Penn, which is that the majority of patients who go into remission stay in remission," said Schuster, who is the senior author on the ASH abstract and is the lead author on the study. The data will be presented at ASH by Richard T. Maziarz, MD, a professor of Medicine at the Oregon Health and Science Knight Cancer Institute.
Two-thirds of DLBCL cases are successfully treated with frontline chemotherapy. When that fails, a high-dose chemotherapy combined with an autologous stem cell transplant can potentially lead to long-term disease-free survival. However, only half of r/r patients are candidates for this approach, and for those who are, the expected three-year event-free survival rate is just 20 percent.
"CAR T therapy represents a potentially life-saving alternative for these patients, who now have a therapy that can help them achieve durable remissions even after other therapies, including transplant, have failed," Schuster said.
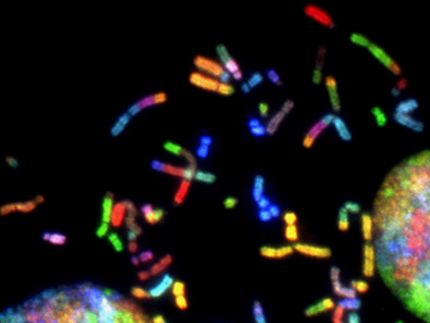
The treatment modifies patients' own immune T cells, which are collected and reprogrammed to potentially seek and destroy the patients' cancer cells. After being infused back into patients' bodies, these CAR-expressing T cells both multiply and attack, targeting cells that express a protein called CD19. Tests reveal that this army of hunter cells can grow to more than 10,000 new cells for each single engineered cell patients receive, producing high remission rates. They can also survive in the body for years.
Grade 3/4 cytokine-release syndrome (CRS), a toxicity associated with CAR T therapy, which includes varying degrees of flu-like symptoms, with high fevers, nausea, and muscle pain, and can require ICU-level care, was reported in 23 percent of patients, 16 percent of whom required treatment with tocilizumab, which is the standard therapy for the toxicity. All patients recovered from their CRS. Other Grade 3/4 toxicities included infections (19 percent of patients), fever resulting from low blood count (15 percent), neurological events (11 percent), and a metabolic abnormality called tumor lysis syndrome (two percent). There were no treatment-related deaths.
Original publication
Alexander E. Perl et al.; "Selective inhibition of FLT3 by gilteritinib in relapsed or refractory acute myeloid leukaemia: a multicentre, first-in-human, open-label, phase 1–2 study"; Lancet Oncology; 2017
Stephen J. Schuster et al.; "Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma"; NEJM; 2018