Chemical 'sponges' designed to soak up toxic cancer-fighting drugs after targeting tumors
Advertisement
Doctors have a powerful arsenal of cancer-fighting chemotherapy drugs to choose from, though a key challenge is to better target these drugs to kill tumors while limiting their potentially harmful side effects.

A view of a sample of a polymer-based membrane material created at Berkeley Lab. The material, which originally had a light-yellow hue, turned red after soaking up a chemotherapy drug.
Roy Kaltschmidt/Berkeley Lab
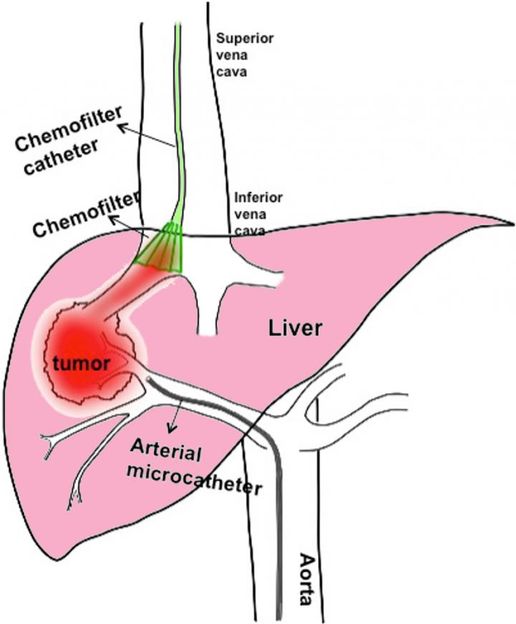
A ChemoFilter device (green) is inserted into a large vein to intercept a chemotherapy drug before it reaches the heart. The drug is delivered to a cancerous tumor in the liver by a tiny tube (middle and bottom) inserted in an artery.
Berkeley Lab

Now, researchers at the Department of Energy's Lawrence Berkeley National Laboratory (Berkeley Lab) are helping to develop and test materials for a new device that can be inserted via a tiny tube into a vein and soak up most of these drugs like a sponge. That's after a separate tube delivers a more concentrated dose to tumors -- and before the drugs can widely circulate in the bloodstream.
Researchers say the drug-capture system could also potentially be applied to antibiotic treatments in combating dangerous bacterial infections while limiting their side effects.
From Fuel Cell to Cancer Treatment
X. Chelsea Chen, a postdoctoral researcher working in the Soft Matter Electron Microscopy program in Berkeley Lab's Materials Sciences Division, had been investigating polymer membranes--which help current to flow in a fuel cell that converts hydrogen and oxygen into electricity -- when she learned about the concept for this new type of medical device.
She saw that the proposed drug-capture device could benefit from the same property in the fuel cell material, which allows it to attract and capture certain molecules by their electric charge while allowing other types of molecules to flow through.
"We used to use this material for transporting protons in a fuel cell," Chen said. "I was really excited when I found out this could be used for chemotherapy -- this was branching out in a totally different direction." The polymer material includes polyethylene, which is strong and flexible and is used for garbage bags, and another polymer containing sulfonic acid, which has a negative electric charge.
Certain types of chemotherapy drugs, such as doxorubicin, which is used to treat liver cancer, have a positive charge, so the polymer material attracts and binds the drug molecules. "In our lab experiments, the current design can absorb 90 percent of the drug in 25-30 minutes," Chen said.
That is important, since an increasingly popular liver-cancer treatment, known as TACE, can allow up to half of the chemotherapy dose to reach the rest of the body even though it is intended to reduce its circulation.
Removing a toxin after tumor treatment
"Doxorubicin has been around for decades. It is very well understood, and it is also very toxic," said Steven Hetts, an associate professor of radiology at UC San Francisco and an interventional neuroradiologist at the UCSF Medical Center who conceived of the new treatment system, called ChemoFilter. "If you get exposed to too much, when it goes through the heart you can go into heart failure." So doctors are very careful with the dose.
Hetts specializes in treating eye tumors by navigating a tube, called a catheter, from the femoral artery in the thigh to the opthalmic artery that supplies blood to the affected eye, and pumping chemotherapy medication through the catheter to the tumor.
"You can get very high concentrations of that chemotherapy in the eye and relatively low concentrations in the rest of the body, but some will wash through the eye and into the veins in the head," Hetts said, "so you can have side effects from that."
Hetts began to question, "Is there a way to drain, to remove that excess drug before it has side effects? If you can remove a lot of the drug, you could escalate the dose of the drug you can give, for better tumor control and potentially a cure -- and you could basically eliminate any side effects.
"It occurred to me that maybe we could navigate a separate catheter into the vein that drains the blood, and have a material that binds up any excess chemotherapy," he said.
While the eye cancers he treats are rare -- there are several hundred children per year in the U.S. who are affected by this kind of tumor--he saw a parallel need to improve the treatment options for liver cancer, which is far more pervasive: It is the third-leading cause of cancer deaths globally, with an estimated half a million new cases each year.
Original publication
Anand S. Patel, Maythem Saeed, Erin J. Yee, Jeffrey Yang, Gregory J. Lam, Aaron D. Losey, Prasheel V. Lillaney, Bradford Thorne, Albert K. Chin, Sheena Malik, Mark W. Wilson, Xi C. Chen, Nitash P. Balsara and Steven W. Hetts; "Development and Validation of Endovascular Chemotherapy Filter Device for Removing High-Dose Doxorubicin: Preclinical Study"; Journal of Medical Devices; 2016