Trojan horses for hospital bugs
Advertisement
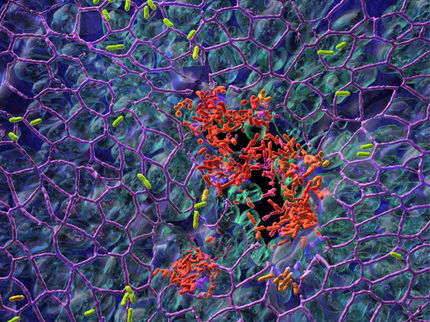
Staphylococcus aureus is a bacterium that is frequently found on the human skin and in the nose where it usually behaves inconspicuously. However, once inside the body, it can have life-threatening consequences such as abscesses, sepsis, pneumonia or myocarditis. How the pathogen manages to perform its disastrous work is still largely in the dark despite intensive research. Scientists from the Universities of Oxford and Würzburg have now unravelled an equally puzzling phenomenon.
WikiImages, pixabay, CC0
Close relatives with distinct differences
"Recent studies have shown that in some cases Staphylococcus strains in the blood of patients differ substantially from those found in the nose," explains Professor Thomas Rudel, Head of the Chair of Microbiology at the University of Würzburg and one of the study's main authors together with his colleague Dr. Martin Fraunholz. "That is astonishing, as both types of bacteria often are very closely related in genetic terms," says Rudel.
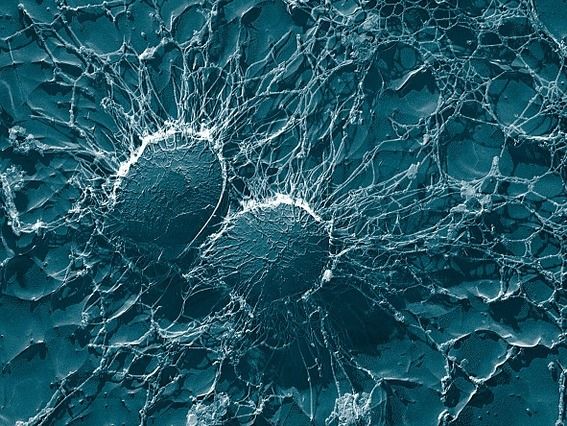
The key differences: These bacteria are much less capable of destroying human immune cells in the blood – compared to their nasal relatives. At the same time, this mutation still allows the bacteria to enter the bloodstream in great numbers, survive much longer, causing a so-called bacteremia.
Differences due to mutation in one gene
In their search for the factor responsible for this loss of dangerous properties, the researchers stumbled upon a specific gene, called rsp in scientific lingo. This gene encodes a transcription factor, i.e. a protein that plays a central role in reading genes and producing proteins. "If the gene is mutated, the properties of the bacteria populating the nose change: their toxicity declines drastically. As a result, bacteria with rsp mutation are absorbed efficiently by the immune system's phagocytes, but they are destroyed after a certain delay only," Rudel further. Being mobile, these immune cells can spread throughout the human body like a Trojan horse, frequently with fatal consequences.
No comparable mutations were found in Staphylococcus strains of the skin. So the scientists draw the conclusion that the new properties are only advantageous when the bloodstream is infected, but not when the skin or other soft tissues are affected.
"Our findings back the suggestion that spontaneous mutations are to blame when the regulatory system based on the rsp transcription factor loses its function," Thomas Rudel sums up the key results of the study. In consequence, the mortality drops at the start of an infection and the modified bacteria can penetrate deeply into the tissues and cause severe diseases. The scientists find this discovery particularly exciting for one reason: It shows that even slight changes to the bacteria's genetic make-up drastically change the pattern and course of the disease. These so-called mutations in the bacteria can even take place while populating humans.