Paradigm shift: 'We need to study lumps of bacteria'
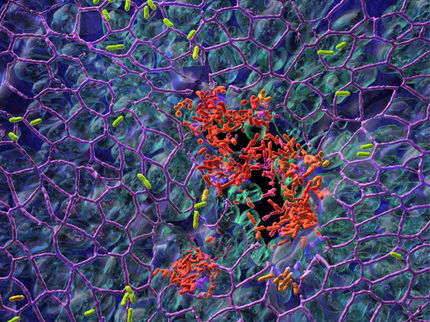
Research from the University of Copenhagen reveals that bacteria which agglutinate before entering the body are far more resistant than single-celled bacteria. This may be the cause of chronic infections.
Since the discovery of bacteria researchers have primarily studied bacteria as organisms that enter the body individually and only then accumulate or agglutinate, creating what is known as biofilm. However, a new study conducted by researchers at the Faculty of Health and Medical Sciences at the University of Copenhagen, among others, indicates that this view of bacteria needs to be revised.
"Bacteria that enter the bloodstream as biofilm are stronger than bacteria that enter the body separately. This is something we have to pay far greater attention to in trying to prevent infections, for example in connection with operations," says Professor Thomas Bjarnsholt from the Costerton Biofilm Center at the University of Copenhagen. He is the senior researcher behind the study.
Biofilm may be the cause of chronic infections. The research team behind the study has examined bacterial environments containing both biofilm and single-celled bacteria.
Here the researchers have found a significantly different type of growth than previously seen. The biofilm takes the main part of the nourishment available and thus outmatches the single-celled bacteria. This makes biofilm the most important player. According to Thomas Bjarnsholt, this is something we need to pay attention, for example when performing operations.
"We have a lot of bacteria on and in our skin which are clustered as biofilm and potentially pathogenic if they enter the skin. In this way biofilm can penetrate or be pushed into the body when the surgeon cuts a hole in the skin containing the biofilm," says Thomas Bjarnsholt.
"Antibiotics are not designed to fight biofilm," says Postdoc Kasper Kragh, who is the main author of the research article. "Often antibiotics are not sufficient to fight chronic infections. This may partly be because antibiotics are to a large extent designed to fight single-celled bacteria, not biofilm."
"We have to take a few steps backwards and, with an open mind, examine how bacteria cause infections and how we can fight them," he adds.
"Hopefully by learning how and when bacteria form biofilm we will be able to find a better way to prevent and treat chronic bacterial infections," concludes Kragh.
Original publication
Original publication
Kasper N. Kragh, Jaime B. Hutchison, Gavin Melaugh, Chris Rodesney, Aled E. L. Roberts, Yasuhiko Irie, Peter Ø. Jensen, Stephen P. Diggle, Rosalind J. Allen, Vernita Gordon, Thomas Bjarnsholt; "Role of Multicellular Aggregates in Biofilm Formation"; mBio; 2016
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.