Next-generation immunotherapy offers new hope for beating brain cancer
Advertisement
High-grade glioma is the most aggressive form of brain cancer. Despite improvements in surgical procedures, chemotherapy, and radiotherapy, this type of brain tumour is still notoriously hard to treat: less than 10% of patients survive beyond five years. Researchers from KU Leuven, Belgium, have now shown that next-generation cell-based immunotherapy may offer new hope in the fight against brain cancer.
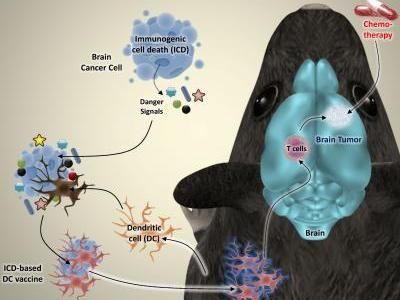
The researchers induced a specific type of cell death in brain cancer cells from mice. The dying cancer cells were then incubated together with dendritic cells, which play a vital role in the immune system. The researchers discovered that this type of cancer cell killing releases 'danger signals' that fully activate the dendritic cells. "We re-injected the activated dendritic cells into the mice as a therapeutic vaccine", Professor Patrizia Agostinis explains. "That vaccine alerted the immune system to the presence of dangerous cancer cells in the body. As a result, the immune system could recognize them and start attacking the brain tumor."
©KU Leuven Laboratory of Cell Death Research & Therapy - Dr. Abhishek D. Garg
Cell-based immunotherapy involves the injection of a therapeutic anticancer vaccine that stimulates the patient's immune system to attack the tumour. Thus far, the results of this type of immunotherapy have been mildly promising. However, Abhishek D. Garg and Professor Patrizia Agostinis from the KU Leuven Department of Cellular and Molecular Medicine have now found a novel way to produce more effective cell-based anticancer vaccines.
The researchers induced a specific type of cell death in brain cancer cells from mice. The dying cancer cells were then incubated together with dendritic cells, which play a vital role in the immune system. The researchers discovered that this type of cancer cell killing releases 'danger signals' that fully activate the dendritic cells.
"We re-injected the activated dendritic cells into the mice as a therapeutic vaccine", Professor Patrizia Agostinis explains. "That vaccine alerted the immune system to the presence of dangerous cancer cells in the body. As a result, the immune system could recognize them and start attacking the brain tumour."
Combined with chemotherapy, this novel cell-based immunotherapy drastically increased the survival rates of mice afflicted with brain tumours. Almost 50% of the mice were completely cured. For the sake of comparison: none of the mice treated with chemotherapy alone became long-term survivors.
"The major goal of any anticancer treatment is to kill all cancer cells and prevent any remaining malignant cells from growing or spreading again", Professor Agostinis continues. "This goal, however, is rarely achieved with current chemotherapies, and many patients relapse. That's why the co-stimulation of the immune system is so important for cancer treatments. Scientists have to look for ways to kill cancer cells in a manner that stimulates the immune system. With an eye on clinical studies, our findings offer a feasible way to improve the production of vaccines against brain tumours."
Original publication
Garg, Abhishek D. and Vandenberk, Lien and Koks, Carolien and Verschuere, Tina and Boon, Louis and Van Gool, Stefaan W. and Agostinis, Patrizia; "Dendritic cell vaccines based on immunogenic cell death elicit danger signals and T cell–driven rejection of high-grade glioma"; Science Translational Medicine; 2016























































