Moffitt develops novel cancer treatment to inhibit chemo-resistance
Despite numerous advances in oncology since the War on cancer began, many patients develop resistance to standard therapies and eventually relapse. Moffitt Cancer Center researchers hope to improve treatment outcomes with development of a novel therapeutic strategy, called adaptive therapy, which is based on evolutionary principals and aims to keep resistant cells in check by maintaining a population of chemo-sensitive cells.
The standard strategy for administering cancer chemotherapy has changed very little over the past five decades. Cancer drug are typically given at the maximum tolerated dose that a patient can tolerate without any life-threatening toxicity. While this strategy works very effectively at killing cancer cells in the short-term, once the chemo-sensitive cells are removed, existing chemo-resistant cells survive and then continue to grow and divide despite the ongoing therapy.
Previously, Moffitt researchers developed a novel treatment strategy based on evolutionary principals and tested originally through mathematical models. Rather than reducing tumor size with a maximum tolerated dose and leaving only resistant cells, the researchers' goal was to prolong survival without disease progression. This strategy, termed an adaptive strategy, uses short bursts of therapy to maintain a residual population of chemo-sensitive cells that keep resistant cells in check and prevent them from growing uncontrollably.
According to Robert Gatenby, M.D., study author and leader of the Cancer Biology & Evolution Program at Moffitt, "there is a natural tendency to use high-dose therapy based on the assumption that each patient receives maximum benefit by killing as many cancer cells as possible. However, according to evolutionary principals, high-dose therapy is the least likely to be successful in controlling the tumor for any length of time because it intensely selects for resistant cells and allows them to grow rapidly because the treatment has eliminated all of their competitors. It is hard to get people to think of an alternative approach in which less therapy might actually be more effective over time. We want to try to work with evolution rather than letting evolution be a source of our defeat."
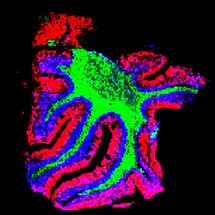
A new article by Gatenby and colleagues published in the Feb. 24 issue of the journal Science Translational Medicine reports that adaptive therapy is effective in preclinical mouse models of triple-negative and ER+ breast cancer. They treated mice with the common breast cancer chemotherapeutic agent paclitaxel according to three different treatment strategies: the standard maximum dose (ST), an adaptive therapeutic dose (AT-1) in which the frequency of paclitaxel is the same but the dose decreases as the tumor responds, and a second adaptive therapeutic dose (AT-2) in which the dose of paclitaxel is the same but doses are skipped when the tumor responds to therapy.
The researchers found that all three treatment strategies initially decreased tumor growth to similar levels; however, as soon as the tumors responded and treatment stopped during the standard regimen or was skipped during the AT-2 regimen, the tumors rapidly regrew. Alternatively, treatment with the AT-1 dosing regimen resulted in a long-term stabilization of the tumor to the point that lower doses of paclitaxel could be used and eventually treatment was able to be withdrawn completely. Mice treated with the AT-1 regimen survived significantly longer than the mice in the standard and AT-2 treatment groups.
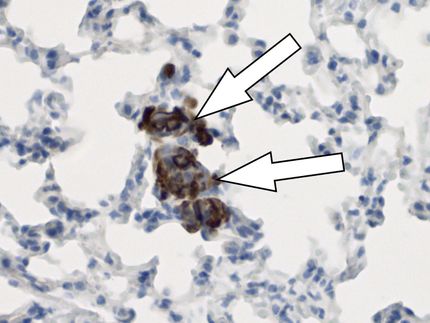
The study showed that adaptive treatment with the AT-1 regimen increases vessel density and blood flow throughout the tumor. This allows chemotherapeutic drugs to be delivered to the tumor more effectively and reduces tumor cell invasion.
Based on these promising preclinical results, Moffitt researchers, led by Jingsong Zhang, M.D., Ph.D., assistant member of the Genitourinary Oncology Program, have initiated the first clinical trial assessing the efficacy of an adaptive treatment strategy in prostate cancer patients. Abiraterone is an inhibitor of androgen synthesis and is typically given to relapsed prostate cancer patients at the maximum tolerated dose. The research team wants to assess if adaptive therapy with abiraterone extends progression-free survival, particularly in African-American men who tend to develop resistance to hormone therapy more rapidly and have a poorer prognosis than other ethnic groups.
A computerized model will be created for each patient to allow individualized treatment based on response to therapy. Patients' PSA levels will be monitored throughout the study and treatment with abiraterone will be stopped and only re-initiated if there is a 50 percent of more increase in the level of PSA.
Gatenby emphasized that "evolving populations can only adapt to the here and now, they can never anticipate the future. But scientists and oncologists can anticipate the future because we understand evolution. Our understanding of evolution is what allows us to develop therapies that could be successfully used in the clinic."
Original publication
Pedro M. Enriquez-Navas, Yoonseok Kam, Tuhin Das, Sabrina Hassan, Ariosto Silva, Parastou Foroutan, Epifanio Ruiz, Gary Martinez, Susan Minton, Robert J. Gillies and Robert A. Gatenby; "Exploiting evolutionary principles to prolong tumor control in preclinical models of breast cancer"; Science Translational Medicine; 2016