What will emerging genetic tools for mitochondrial DNA replacement mean for patients?
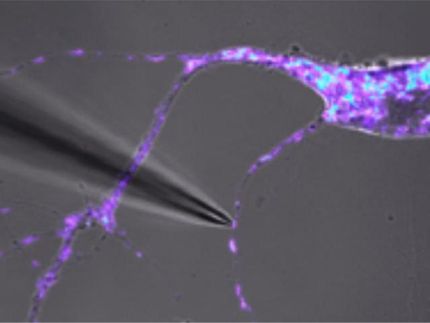
Sophisticated prenatal techniques, not yet in clinical practice, offer the potential to prevent a cruel multi-system genetic disease passing from mother to child long before birth.
But these emerging tools raise important questions: might there be unintended, even irreversible risks to the resulting child--or even that child's future descendants? Are there potential risks to the mother's health? What about other potential consequences if its use is broadened to include indications beyond strict disease prevention, such as adapting the tools into conception aids for older women?
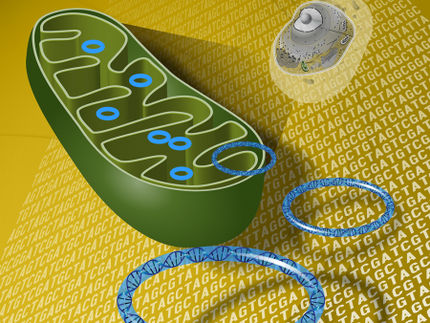
The tools in question, mitochondrial replacement techniques (MRTs), aim to prevent mother-to-child transmission of mitochondrial DNA disease --a complex set of rare disorders caused by defective DNA within the mitochondria, the tiny energy-producing structures existing outside the nucleus of cells. Such disease may present at any age or level of severity, attacking a combination of organs and systems, often fatally. There are no current cures or approved therapies for any of these disorders, which clinicians manage by treating the diverse symptoms that may progressively affect each patient.
Earlier this month, an expert panel of national experts formed by the Institute of Medicine at the request of the U.S. Food and Drug Administration (FDA) recommended that research into MRTs should proceed under carefully proscribed guidelines.
"Even though MRTs would not confer health benefits on patients who already have mitochondrial DNA diseases, many patients with a known risk for transmitting such a disease to their offspring are highly motivated to prevent that from occurring," said Marni J. Falk, M.D., director of the Mitochondrial-Genetics Clinic at The Children's Hospital of Philadelphia and first author of the article. "That motivation is clear when we counsel patients and families affected by mtDNA disease, and recent patient surveys have reinforced that preventing disease transmission is a prevailing concern in this population."
Falk's co-authors are Jeffrey Kahn, Ph.D., M.P.H., of the Johns Hopkins Berman Institute of Bioethics, and Alan Decherney, M.D., an obstetrician-gynecologist and reproductive endocrinologist at the National Institute of Child Health and Human Development. Kahn chaired the Institute of Medicine expert panel.
Because the expert panel stated that the child's safety was paramount, it recommended that MRTs should initially be studied only in male embryos, since males do not transmit mitochondrial DNA to their children. The panel further argued that the FDA should make clear policy and that professional societies should issue practice recommendations to limit future MRT usage to appropriate patients.
The authors repeat the panel's stipulation that children conceived after MRT should be monitored long-term, "probably well into adulthood," much longer than is done after in vitro fertilization with pre-implantation diagnosis for diseases based in nuclear DNA.
Finally, because MRTs require mixing mitochondrial DNA from a female donor with DNA from the nucleus of the mother and father, the authors note that researchers should investigate unanticipated health problems and possibly questions about identity, before regulatory approval or clinical use can occur for the techniques.
Original publication
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.