Immune system cells key to maintaining blood-brain barrier
New research shows that the cells responsible for protecting the brain from infection and inflammation are also responsible for repairing the system of defenses that separates the brain from the rest of the body. These findings have significant clinical implications because certain cardiovascular drugs could possibly impede the brain’s ability to repair itself after a stroke or other injury.
“This study shows that the resident immune cells of the central nervous system play a critical and previously unappreciated role in maintaining the integrity of the blood-brain barrier,” said Maiken Nedergaard, M.D., D.M.Sc. , co-director of the Center for Translational Neuromedicine at the University of Rochester Medical Center (URMC) and lead author of the study. “When this barrier is breached it must be rapidly repaired in order to maintain the health of the brain and aid in recovery after an injury – a process that could be impaired by drugs that are intended to prevent this damage in the first place.”
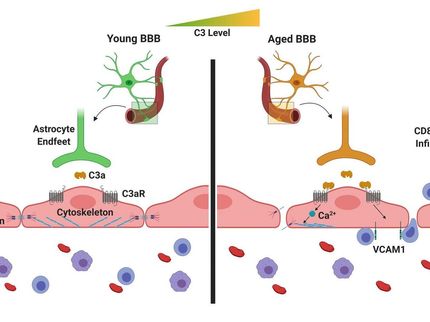
The brain is essentially an independent and separate ecosystem. It possesses a dedicated system of defenses against infection and recently Nedergaard and her colleagues demonstrated that the brain also maintains its own unique process of removing waste . Movement in and out of the brain is tightly controlled through a complex system of gateways and controls that are collectively referred to as the blood-brain barrier (BBB).
When the BBB is breached the brain becomes vulnerable to infection and injury. It is, therefore, imperative that the openings in the BBB are resealed, and quickly. This most frequently occurs during a stroke, which triggers inflammation that can cause the BBB to break down.
The new study reveals that the brain’s immune system, specifically cells called microglia, play a central role in the process of repairing damage to the BBB.
Microglia serve as the brain’s “first responders” and are present throughout the brain and spinal cord. These cells are constantly monitoring their environment, and can be switched on or activated to perform different functions such as control inflammation, destroy pathogens, clean up the debris from dead or damaged cells, and seal off the site of an injury.
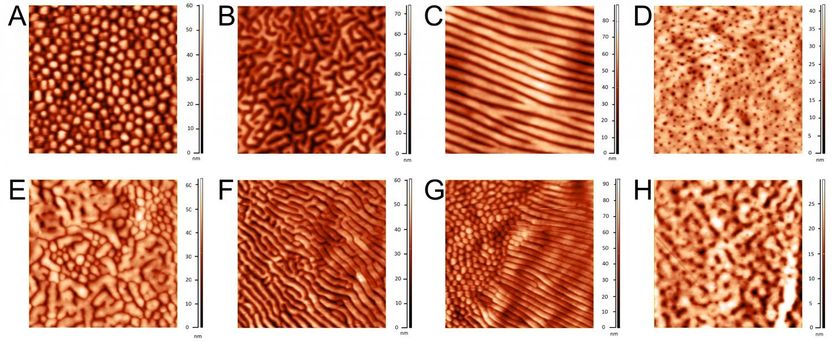
Performing experiments in mice, Nedergaard and her colleagues observed that when small holes where made in the BBB, nearby microglia were rapidly mobilized and set about repairing the breach. In most instances, the integrity of the BBB was restored within 10 to 30 minutes.
The team identified a receptor called P2RYX12 that was responsible for activating the microglia and directing them to the site of the damage. This finding is significant because the same receptor is also present on platelets and is one of the targets of blood thinning drugs such as Plavix.
These drugs are given to individuals at risk of heart attack and stroke and helps prevent platelets from binding together to form blood clots that, when they make their way to the brain, can block the flow of blood and trigger a stroke. However, because these drugs also suppress P2RYX12 receptors in microglia, they could potentially impair the ability of the brain to carry out repairs to the BBB once a stroke occurs.
Nedergaard and her team are currently investigating the impact of P2RYX12-blocking drugs on microglia function in the brain.
“Our concern is that while certain types of blood thinning drugs may do a great job preventing strokes, they could have the unintended consequence of making them worse or hindering recovery once they occur,” said Nedergaard.
Original publication
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
More news from our other portals
Last viewed contents
Cytogen to Raise $20 Million Through Private Placement of Common Stock and Warrants
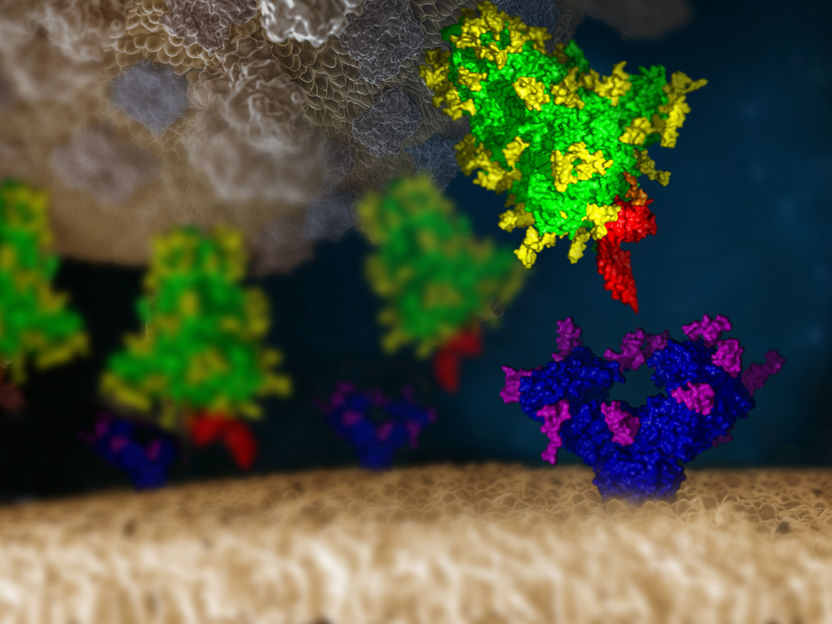
Neutralizing the SARS-CoV-2 sugar coat - Researchers may have found the “Achilles’ heel” of the virus