Powerful protein promotes post-injury regeneration and growth of injured peripheral nerves
The peripheral nervous system is a vast network of nerves that exists primarily outside of brain and spinal cord and connects to the far reaches of the body. The very expanse of peripheral nerves makes them highly vulnerable to injuries such as blunt-force blows, cuts, and leg and arm fractures, as well as diseases that attack peripheral nerves such as diabetes, Charcot-Marie-Tooth, and Guillain-Barre syndrome. Unlike the central nervous system (brain and spinal cord), peripheral nerves do have the capacity to regenerate, and inflammatory immune responses play a key role in regeneration.
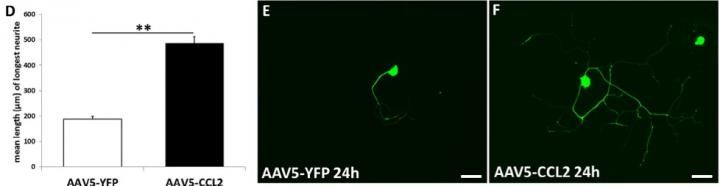
In part D the average length of the longest neurite from >250 neurons after 24 hours in culture. Parts E and F show an example of an individual nerve cell from each condition.
Case Western Reserve University School of Medicine
Case Western Reserve University School of Medicine scientists have demonstrated in lab animals the regenerative dynamics of a specific signaling protein, C-C class chemokine 2 (CCL2). CCL2 sends inflammatory immune cells (macrophages) to peripheral nerve cell clusters to promote repair and to trigger gene expression that leads to new growth in nerve cells.
"We are excited about our findings because we had no reason to expect that just expressing the chemokine CCL2 would be enough to stimulate nerve regeneration," senior author Richard E. Zigmond, PhD, professor of Neurosciences and Pathology, Case Western Reserve University School of Medicine. "It is remarkable that CCL2 should be so powerful."
Post-injury, CCL2 affects the workings of peripheral nerve cell clusters, known as ganglia, and the nerve fibers distal to the site of injury. Each peripheral nerve cell has a main body and a tail-like extension, known as an axon. For sensory nerve cells, the axon splits after leaving the cell body, with one part projecting from the nerve cell body to capture sensations, while the other forwards the information to the spinal cord and brain.
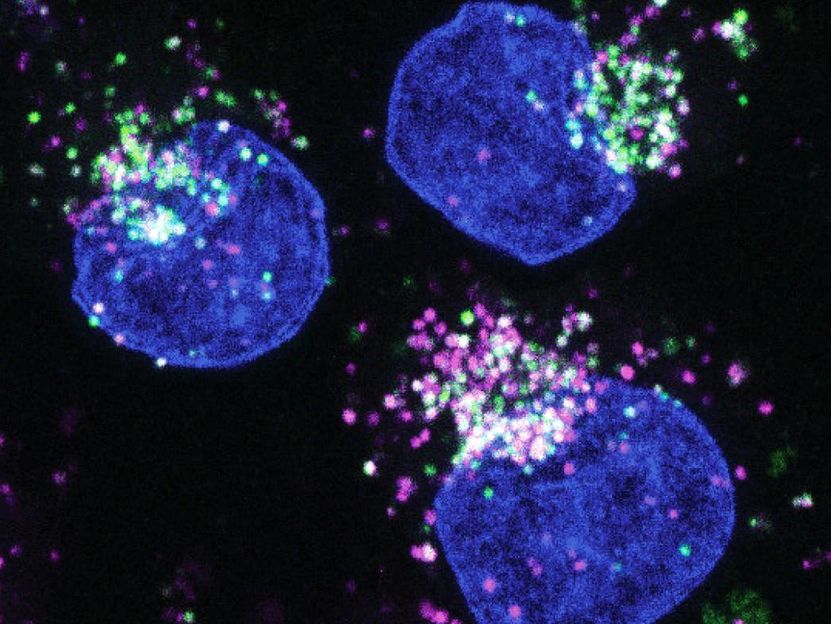
After an injury to a region of peripheral nerves, CCL2 signals macrophages to move to the damaged areas of axons and remove cellular debris, clearing the way for new axon growth. CCL2 also signals macrophages to enter into the injured ganglia regions that house individual nerve cells to promote nerve regeneration as well. At least in part, regeneration also occurs because macrophages trigger genes that promote new axon growth.
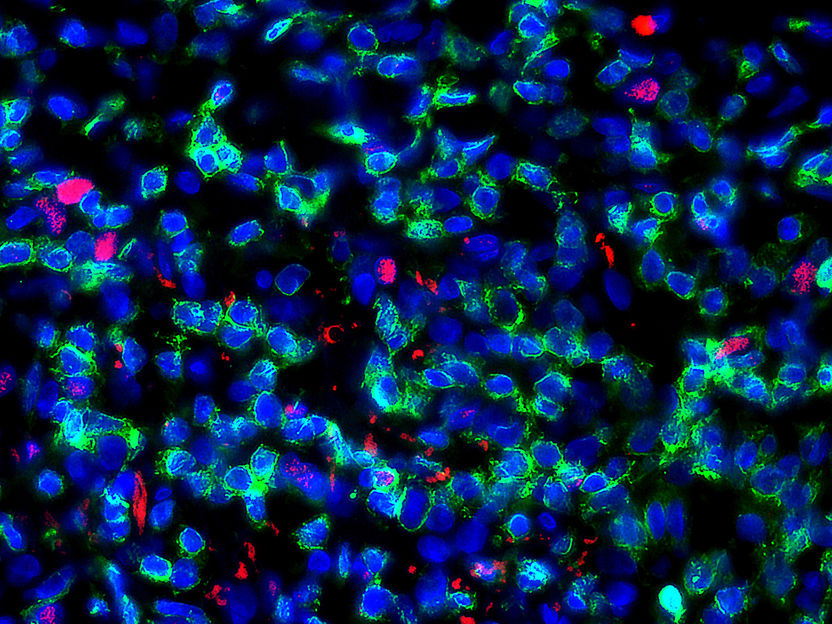
Zigmond's most recent study demonstrated the workings of this CCL2 mechanism in lab animals. In one experiment, senior graduate student Jon Niemi injected into wild-type, uninjured mice a virus designed to trigger CCL2 expression. The boost in CCL2 expression in these mice led to greater accumulation of macrophages three weeks later in dorsal root ganglia, a cluster of sensory nerve cells that project both to peripheral areas and to the central nervous system. More macrophage build-up, in turn, produced greater neuron sprouting, the beginnings of nerve regeneration.
However, the experience was entirely different in another set of mice lacking a receptor (CCR2) that enables CCL2 to act. Without the receptor, the same spike in macrophage accumulation simply did not occur in CCR2-deficient mice. These animals only had scant nerve growth that did not nearly match the nerve regeneration observed in wild-type mice.
"We did the same experiments in another type of mouse and found the same correlation," Zigmond said. "If macrophages don't come into the ganglia, then regeneration is substantially impeded. We found this true of sensory and sympathetic neurons. We concluded that there was a correlation between macrophage entry into ganglia and nerve regeneration."
The researchers also demonstrated the role of CCL2 overexpression in altered gene expression.
Investigators tested for changes in the expression of certain genes by screening mRNA molecules associated with nerve regeneration in the animals where CCL2 overexpression prompted neuron outgrowth. Changes in one mRNA and one protein emerged -- leukemia-inhibitory factor (LIF) mRNA and neuronal pSTAT3 (signal transducers and activators of transcription 3). These special molecules act on cells by expressing genes important to instructing neurons to grow. By causing macrophage accumulation, CCL2 increases levels of LIF mRNA and pSTAT3, which leads to an increased regenerative capacity of dorsal root ganglia neurons. To test their hypothesis, the group blocked the activation of LIF signaling using inhibitors of STAT3 activation. Inhibiting STAT3 activation did not result in an increase in neurite growth, despite an increase in CCL2 that would normally increase growth of dorsal root ganglia neurons.
The findings by Zigmond and fellow investigators shed a new light on inflammation. Rather than fight inflammation at the very outset of a peripheral nerve injury, perhaps allowing limited inflammation post-injury may be therapeutic in stimulating neuron regeneration. These findings about CCL2 could also have implications for illnesses that affect peripheral nerves.
"Our conclusion is that the immune system and the nervous system are interacting in a beneficial way to create macrophage-induced inflammation and promote nerve regeneration," Zigmond said. "This is occurring around the cell bodies. There is something happening within the cell in response to macrophage activity, in addition to macrophage action on to the damaged distal nerve axon."
Joining Zigmond and lead author Niemi in this research were contributing authors Alicia DeFrancesco-Lisowitz, Jared Cregg, and Madeline Howarth, all of the Department of Neurosciences, Case Western Reserve University School of Medicine.
Original publication
Jon P. Niemi, Alicia DeFrancesco-Lisowitz, Jared M. Cregg, Madeline Howarth, Richard E. Zigmond; "Overexpression of the monocyte chemokine CCL2 in dorsal root ganglion neurons causes a conditioning-like increase in neurite outgrowth and does so via a STAT3 dependent mechanism"; Experimental Neurology; 2015