When bowels and brain are out of sorts
Gastrointestinal disorders are often linked to psychological dysfunctions and can be explained by a malfunction of the communication between bowels and brain, as has been shown by a research project funded by the Austrian Science Fund FWF.
According to estimates, one in five individuals suffers from recurring abdominal cramps, a sense of fullness, digestive problems or irritable bowel syndrome (IBS), but in most cases no cause can be identified. In a recently completed project funded by the Austrian Science Fund FWF, a research team from Graz headed by Peter Holzer investigated the impact of chronic inflammatory abdominal pain on the brain’s functioning and on social behaviour. In animal tests, the scientists were able to demonstrate marked changes in the brain linked both to (pain) memory and emotions.
Brain function and behaviour
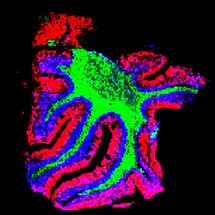
Peter Holzer and his team took a closer look at the two aspects of pain sensitivity and stress. Their investigations showed that colitis will increase pain sensitivity and thus have an impact on the brain. This, in turn, will influence the social behaviour of the affected individuals, leading, for instance, to withdrawal or anxiety disorders. “Behavioural changes caused by colitis are reflected in the limbic system and the connected regions of the cortex”, explains Peter Holzer and notes that chronic abdominal pain is often connected to psychopathologies. Therefore it is particularly important to include these accompanying disorders in the examination. If stress is involved, the researchers assume this might increase pain sensitivity. It has been shown that this is not true for low-level, “predictable” stress. In that case the resistance against visceral pain stimuli is even increased, as the impact of the stressful situation on brain functions has proven.
Looking for connections
Attempts to get to the bottom of the complex phenomenon of chronic (abdominal) pain can be likened to the work of a detective and often leads away from the actual trigger to other bodily functions. Accordingly, researchers increasingly try to understand the interaction of different body systems. In the case of abdominal pain, studies have hitherto focused on the very pain-sensitive nervous fibres present in the gastrointestinal tract. After all, a total of five nervous systems run through the digestive tract. “Many interesting angles have been found and drugs developed. But in clinical tests in patients, the medication turns out to have little or no effect”, Holzer tells us. “The lesson to be learned from this: chronic abdominal pain is not only produced by an oversensitivity of nerves in the gastro-intestinal tract, but something else has to be involved that is closer to the brain.”
A multitude of information and pathways
Scientists are becoming increasingly clear as to how much information is actually passed from the intestines to the brain in cases of abdominal pain. The current FWF research project proves that it is not only the neural pathways that are of significance here, but also hormonal and immunological signalling pathways. In addition, there is the latest research on the gut microbiome, the intestinal eco-system with its multitude of bacteria. “Gut microbiota have an impact on all sorts of bodily functions, including the brain and pain sensitivity, and also the individual’s mood”, says Holzer. In the context of the MyNewGut EU project, researchers from the Medical University of Graz are investigating whether the composition of the gut microbiota has an impact on brain function. “For a comprehensive understanding of chronic pain syndromes it is important to take into account all information pathways, not only the neuronal ones, between the periphery and the brain”, Holzer stresses. The expert is convinced that only a normalisation of disturbed brain functioning could lead to a successful therapy for chronic pain.
Original publication
Piyush Jain, Ahmed M. Hassan, Chintan N. Koyani, Raphaela Mayerhofer, Florian Reichmann, Aitak Farzi, Rufina Schuligoi, Ernst Malle and Peter Holzer, Behavioral and molecular processing of visceral pain in the brain of mice: impact of colitis and psychological stress; Frontiers in Behavioral Neuroscience, July 2015
Ahmed M. Hassan, Piyush Jain, Florian Reichmann, Raphaela Mayerhofer, Aitak Farzi, Rufina Schuligoi and Peter Holzer; Repeated predictable stress causes resilience against colitis-induced behavioral changes in mice; Frontiers in Behavioral Neuroscience, November 2014
Peter Holzer and Aitak Farzi; Neuropeptides and the Microbiota-Gut-Brain Axis; Microbial Endocrinology: The Microbiota-Gut-Brain Axis in Health and Disease, June 2014