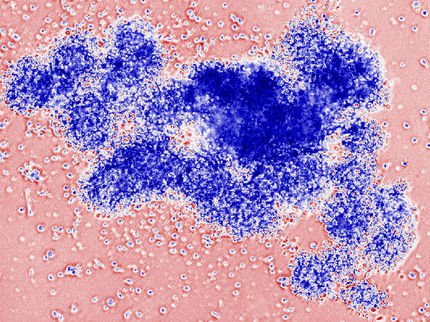
High-fat diet accelerated heart transplant rejection in mice
Hyperlipidemia, Caused by a High-Fat Diet, Aggressively Accelerates Organ Rejection
In two studies published online today in the American Journal of Transplantation, researchers determined that hyperlipidemia accelerates heart-transplant rejection in mice. By using models that mimic the health conditions found in human transplant recipients, the researchers from Tufts determined that transplant rejection was accelerated whether the hyperlipidemia (high cholesterol and high triglycerides in the blood) was caused by genetics or solely by a high-fat diet.
“Our work fundamentally changes how we view transplant rejection. The common cause of transplant rejection in these mice was a high-fat diet. We also demonstrate that the canonical understanding of organ rejection is not complete,” said senior author John Iacomini, Ph.D., professor in the department of developmental, molecular, and chemical biology at Tufts University School of Medicine and a member of the genetics and immunology program faculties at the Sackler School of Graduate Biomedical Sciences at Tufts.
Mice fed a high-fat diet rejected their heart transplants faster than mice fed a lower-fat diet. Transplanted hearts lasted in four groups of mice as follows:
- 21 days: mice with hyperlipidemia caused by a genetic mutation of apolipoprotein E (ApoE) placed on a high-fat diet
- 51 days: healthy mice placed on a high-fat diet leading to hyperlipidemia
- 61 days: mice with hyperlipidemia caused by a genetic mutation of ApoE on a lower-fat diet
- More than 100 days: healthy mice placed on a lower-fat diet
Mice were on the high-fat or lower-fat diet for four weeks before transplantation and maintained on the same diet after transplantation.
“We used mice with conditions that mimic those often found in transplant patients — hyperlipidemia is common in patients before transplantation but can also be caused by drugs to prevent organ rejection — and discovered that it accelerates organ rejection. The main problem for patients is rejection, so if organ rejection can be controlled, survival increases,” said co-first author, Jin Yuan, M.D., Ph.D., postdoctoral scholar in the department of developmental, molecular, and chemical biology at Tufts University School of Medicine and member of Iacomini’s laboratory.
“Most of our understanding of transplant rejection comes from work done over the past 50 years using healthy animal models. It led us to believe that transplant rejection is caused by a type of T helper cell called Th1. This is the canonical understanding of organ rejection. We found, however, that increased levels of another type of T helper cell, known as Th17, are partially responsible for accelerated heart-transplant rejection in mice with hyperlipidemia. Hyperlipidemia also affects regulatory T cells and disrupts their ability to prevent transplant rejection,” said co-first author, Jessamyn Bagley, Ph.D., assistant professor of medicine at TUSM and member of Iacomini’s laboratory.
“Hyperlipidemia is a common condition in heart-transplant recipients, and the effects of it —while not closely studied previously — are of major relevance to how we treat rejection and warrant further examination. The data from our two studies provide the evidence we need to begin examining whether similar changes are observed in humans with hyperlipidemia. If so, it may be possible to improve transplant outcomes by altering diets and developing therapies that target the specific cells altered by this condition,” said Iacomini.
The studies are accompanied by an editorial entitled “Do Mice Need an Order of Fries to be Relevant for Transplant Studies?” by Jonathan Maltzman, M.D., Ph.D., and Deirdre Sawinski, M.D., both of the Perelman School of Medicine at the University of Pennsylvania.
“By feeding mice the equivalent of fried food, the studies by Iacomini and his team might be more applicable to humans than the majority of studies to date, which have used mice without the conditions that plague many of our human transplant recipients,” said Maltzman.
“The studies clearly show that a high-fat diet with or without the genetic loss of ApoE can alter the immune response in mice after heart transplantation,” he continued.
Original publication
Yuan, J., Bagley, J., and Iacomini, J.; "Hyperlipidemia promotes anti-donor Th17 responses that accelerate allograft rejection."; American Journal of Transplantation 2015.
Bagley, J., Yuan, J., Chandrakar, A., and Iacomini, J.; "Hyperlipidemia alters regulatory T cell function and promotes resistance to tolerance induction through costimulatory molecule blockade."; American Journal of Transplantation 2015.