New Molecular Diagnostic Methods Could Reduce Risk of Miscarriage in Prenatal Testing for Genetic Diseases
Early diagnosis and treatment are crucial to improving patient prognosis for 22q11 deletion syndrome and Wilson’s disease, two potentially life-threatening genetic conditions. Breaking research in Clinical Chemistry, the journal of AACC, shows for the first time that a more precise technology for quantifying DNA could enable all newborns to be tested for 22q11 deletion syndrome; and that a new method known as cSMART can diagnose a fetus with Wilson’s disease without the risk of miscarriage that comes with traditional prenatal tests.
22q11 deletion syndrome is considered one of the most common chromosomal deletions associated with birth defects and leads to a wide range of health problems, from heart defects to behavioral disorders. Proposals have been made to include 22q11 deletion syndrome in newborn screening panels so that infants can be diagnosed and treated immediately after birth. The current gold standard method for diagnosing this disorder, however, is too expensive and labor-intensive for screening all newborns.
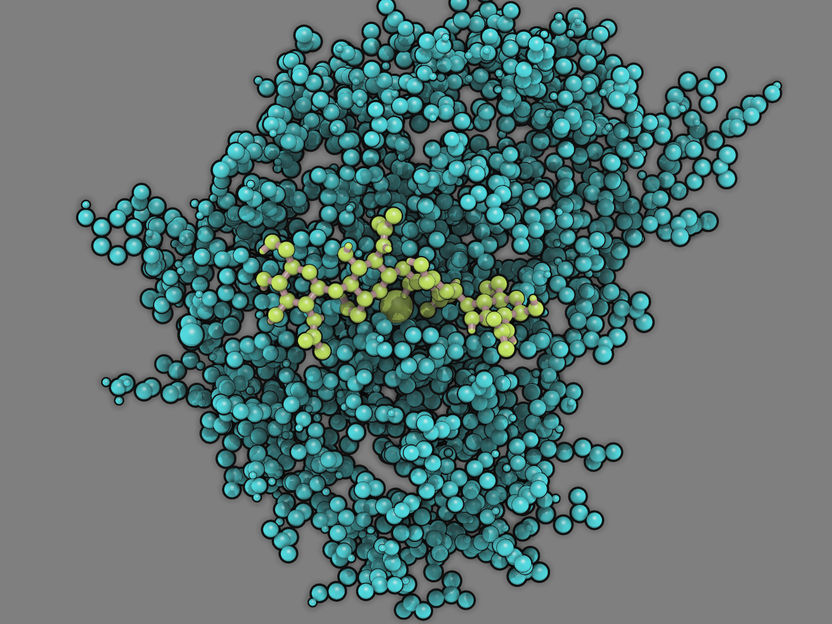
A team of researchers led by Flora Tassone, PhD, of the University of California Davis Medical Center, Sacramento, California, has now shown for the first time that a method for quantifying DNA known as droplet digital polymerase chain reaction (ddPCR) can reliably and cost-effectively diagnose 22q11 deletion syndrome. To determine this, the researchers blindly intermixed blood spot cards (the sample form used in newborn screening) from 26 22q11 deletion syndrome patients with 1,096 cards from the general population. Using ddPCR to analyze each sample, they were able to correctly identify the 26 cases of 22q11 deletion syndrome with 100% accuracy and at a cost of only $5–6 for reagents per reaction.
Wilson’s disease results from a mutated version of the gene ATP7B that when inherited from both parents causes liver and neurological damage and eventual death. If detected and treated early enough, however, patients with Wilson’s disease can lead normal lives. Currently, prenatal diagnosis of Wilson’s disease is performed by analyzing fetal cells collected by either chorionic villus sampling or amniocentesis. Both of these invasive methods come with the risk of complications such as miscarriage, but Wilson’s and other single-gene disorders like it are difficult to diagnose using safer non-invasive methods—which analyze fetal DNA in the mother’s blood—because the fetal gene of interest is present in the mother’s blood at such low levels.
A team of researchers led by Lingqian Wu, PhD, of Central South University, Hunan, China, has now developed a new non-invasive prenatal testing method named circulating single-molecule amplification and resequencing technology (cSMART). In a study of four pregnancies where both parents were Wilson’s disease carriers, Wu’s team demonstrated that cSMART can diagnose Wilson’s disease if the sequences of the parents’ mutant ATP7B variants are known. The researchers used DNA sequencing to determine each couple’s ATP7B variants, then used both standard invasive prenatal testing and cSMART to test for these respective variants in each couple’s baby. Among the four pregnancies, invasive prenatal testing detected two carrier fetuses who had inherited mutant paternal ATP7B, one unaffected fetus, and one fetus with Wilson’s disease. cSMART successfully made the exact same diagnoses.
Other news from the department science
Most read news
More news from our other portals
See the theme worlds for related content
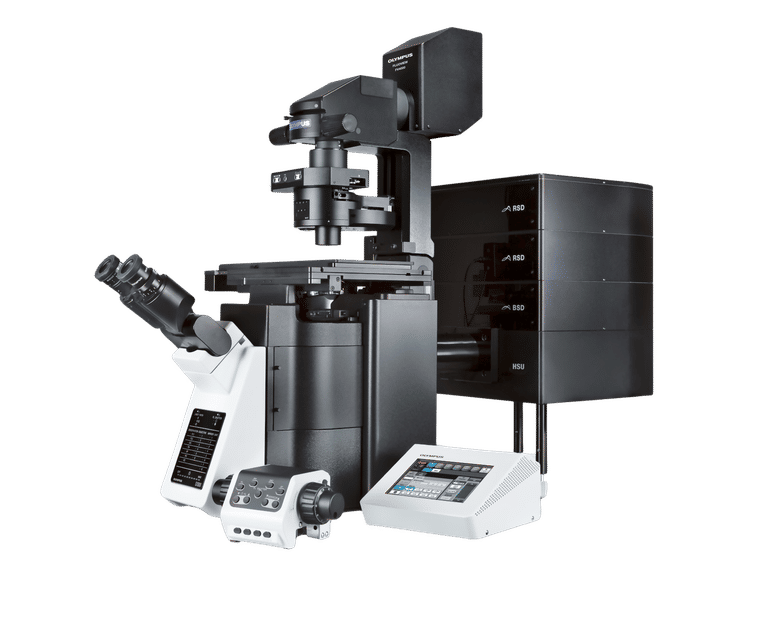
Topic World PCR
This groundbreaking and highly versatile molecular technique of PCR allows us to amplify tiny amounts of genetic material on a large scale and analyze them in detail. Whether in medical diagnostics, forensic DNA analysis or research into genetic diseases - PCR is an indispensable tool that gives us deep insights into the world of DNA. Immerse yourself in the fascinating world of the polymerase chain reaction (PCR)!
Topic World PCR
This groundbreaking and highly versatile molecular technique of PCR allows us to amplify tiny amounts of genetic material on a large scale and analyze them in detail. Whether in medical diagnostics, forensic DNA analysis or research into genetic diseases - PCR is an indispensable tool that gives us deep insights into the world of DNA. Immerse yourself in the fascinating world of the polymerase chain reaction (PCR)!