New version of common antibiotic could eliminate risk of hearing loss
On Christmas Eve, 2002, Bryce Faber was diagnosed with a deadly cancer called neuroblastoma. The 2-year-old's treatment, which, in addition to surgery, included massive amounts of radiation followed by even more massive amounts of antibiotics, no doubt saved his life. But those same mega-doses of antibiotics, while staving off infections in his immunosuppressed body, caused a permanent side effect: deafness.
"All I remember is coming out of treatment not being able to hear anything," said Bryce, now a healthy 14-year-old living in Arizona. "I asked my mom, 'Why have all the people stopped talking?'" He was 90 percent deaf.
Treatment with aminoglycosides, the most commonly used class of antibiotics worldwide, is often a lifesaving necessity. But an estimated 20-60 percent of all patients who receive these antibiotics suffer partial or complete hearing loss.
Now, in a study that will be published in the Journal of Clinical Investigation, researchers at the Stanford University School of Medicine report that they have developed a modified version of an aminoglycoside that works effectively in mice without the risk of causing deafness or kidney damage, another common side effect. The researchers hope to test versions of the modified antibiotic in humans as soon as possible.
"If we can eventually prevent people from going deaf from taking these antibiotics, in my mind, we will have been successful," said Anthony Ricci, PhD, professor of otolaryngology-head and neck surgery and co-senior author of the study. "Our goal is to replace the existing aminoglycosides with ones that aren't toxic."
Four years in the making
It took the scientists four years of research to produce 5 grams of the newly patented antibiotic, N1MS, which is derived from sisomicin, a type of aminoglycoside.
N1MS cured urinary tract infection in mice just as well as sisomcicin, but did not cause deafness, study results show. The study presents a promising new approach to generating a new class of novel, nontoxic antibiotics, Ricci said.
The two senior authors - Ricci and Alan Cheng, MD, associate professor of otolaryngology-head and neck surgery - joined forces in 2007 to explore the idea of creating new and improved versions of these antibiotics based on a simple yet groundbreaking idea born of Ricci's basic science research into the biophysics of how hearing works within the inner ear.
"It's a nice example of how basic science research is directly translatable into clinical applications," said Ricci.
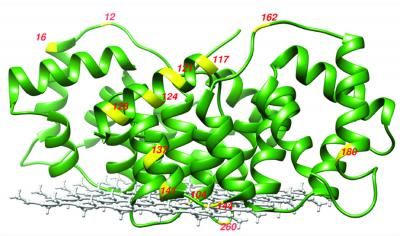
Ricci is an expert on the process by which sound waves open ion channels within the sensory hair cells of the inner ear, allowing their conversion to electrical signals that eventually reach the brain.
Because aminoglycosides cause deafness by killing these nonregenerating hair cells, Ricci postulated, why not simply make the drug molecules unable to enter the cells' channels?
The idea made sense to Cheng.
"As a clinician-scientist, I treat kids with hearing loss," Cheng said. "When a drug causes hearing loss it is devastating, and it's especially disturbing when this happens to a young child as they rely on hearing to acquire speech.
"When I came to Stanford seven years ago from the University of Washington, I was exploring the angle that maybe we could add drugs to protect the ear from toxicity. Tony brought up this new idea: Why don't we just not let the drug get in? Great idea, I thought. When do we start to work?"
Most read news
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
New tool for studying membrane protein structure
Category:Biodiesel_producers
National_Coalition_for_Cancer_Survivorship


















































