Bacterial defense policies
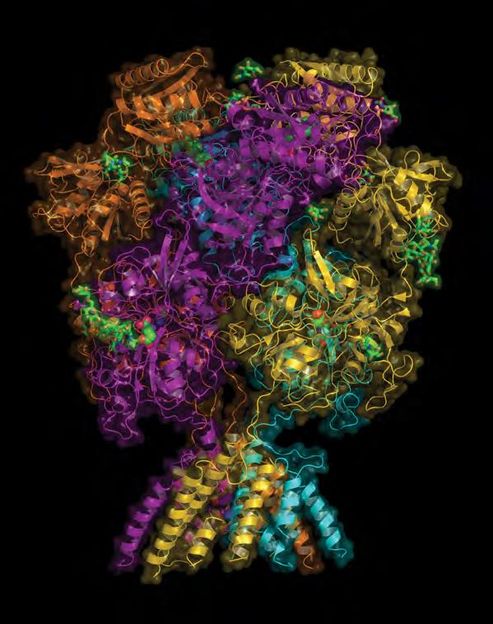
High-resolution cryo-electron microscopy has now revealed in unprecedented detail the structural changes in the bacterial ribosome which results in resistance to the antibiotic erythromycin.
Multiresistant bacterial pathogens that are insensitive to virtually all available antibiotics are one of the major public-health challenges of our time. The question of how resistance to various antibiotics develops is the focus of research being carried out by LMU biochemistDaniel Wilsonand his colleagues. As they report in the journal Molecular Cell, he and his team have used high-resolution cryo-electron microscopy to obtain novel insights into the ultrastructural changes in an intracellular machine associated with the acquisition of resistance to the antibiotic erythromycin. “A better understanding of this mechanism is an important step towards the development of new and more potent antibiotics,” Wilson says.
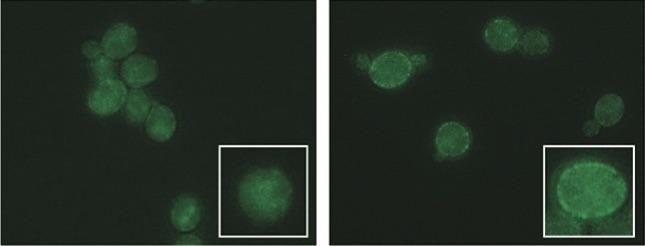
Erythromycin targets bacterial ribosomes – the nanomachine responsible for the translation of messenger RNA (mRNA) sequences into protein – thus preventing synthesis of the proteins required for continued growth and survival. Bacteria can become resistant to the antibiotic either as the result of a spontaneous mutation or by picking up an appropriate “resistance gene” (which codes for a protein that confers resistance) from another bacterium via genetic exchange. However, as Wilson explains: “The genes necessary for resistance are often activated only when required (i.e., when the antibiotic is present in the environment), and so-called leader or signal peptides play an important role in this process.” The leader peptides regulate the expression of the downstream resistance gene in response to the presence of the drug. When the drug is present, it binds within the tunnel of the ribosome and interacts with the translating leader peptide to stall protein synthesis. The drug-induced stalling allows for a change in the structural conformation of the mRNA, which in turn, unmasks a ribosome-binding site downstream, enabling the nucleotide sequence that encodes the resistance factor itself to be translated.
Diverse ways of gumming up the works
“Exactly how the interaction between antibiotic and leader peptides occurs at the structural level, so as to cause the ribosome to stall, has remained unclear,” Wilson says. The researchers had previously shown that the signal peptide encoded by the ermBL mRNA does not interact directly with erythromycin. Instead, the signal peptide adopts a specific conformation in the presence of the antibiotic, which blocks and inhibits the active center of the ribosome, thus accounting for the premature stop. “Since there are other signal peptides apart from the ErmBL leader, we were interested in finding out whether they make use of this same mechanism or have different modes of action,” Wilson explains. In their new study, the researchers took advantage of a recent technological breakthrough: “Thanks to the use of a new detector, we were able to increase the resolution of our structures from 4.5 Å to 3.5 Å, which makes previously hidden details visible,” says Wilson.
The new analyses revealed that the ErmCL leader peptide employs quite a different mechanism to signal the presence of the antibiotic. Unlike its ErmBL counterpart, the ErmCL signal peptide interacts directly with the antibiotic. As a consequence, at a certain point during translation, the conformation of the ribosome’s active site is distorted in such a way that further elongation of the nascent peptide becomes impossible. Wilson is convinced that a thorough understanding of such antibiotic-sensing mechanisms will stimulate the development of more effective antibiotics in the future. He and his group now plan to enhance still further the resolution attainable with their cryo-electron microscope, and will then use it to investigate the structures of ribosomes that have been brought to a halt by other chemical agents.