Treating gastric cancer -- with Botox
Cutting the signals sent to cancer stem cells suppressed their growth
Researchers have found a novel approach to treating cancer - using Botox. A study presented in the 20 August edition of Science Translational Medicine shows that cancer growth could be suppressed by eliminating the signals sent by nerves that are linked to cancer stem cells. The approach thus treated the cancer. The use of Botox made the treatment cheap, safe and efficient. The researchers have thus far tested the procedure on mice, and will soon start testing on humans.
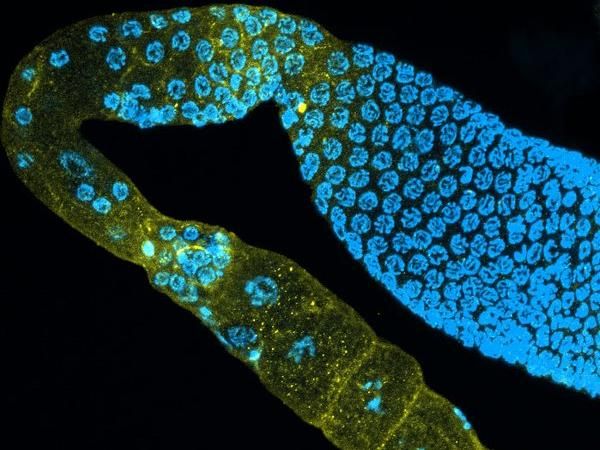
The nervous system is crucial in regulating many organs. Researchers from the Norwegian University of Science and Technology (NTNU), Columbia University and MIT, along with researchers from Japan and Germany have now shown that the vagal nerve contributes to the growth of gastric tumors, so that stopping the nerve signal to the tumor will stop its growth.
"This study shows that nerves control cancer stem cells," say NTNU Professor Duan Chen and Columbia Professor Timothy Wang, the co-corresponding authors of the study published in this week's edition Science Translational Medicine.
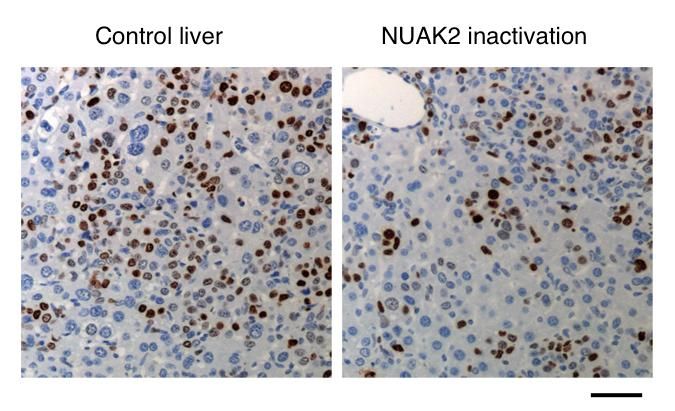
"We found that by removing the effect of the nerve, the stem cells in the cancer tumor are suppressed, leading to cancer treatment and prevention," Chen said.
This study found that nerves promote tumor growth through the release of a neurotransmitter.
The researchers tried four methods to cut the connection between the nerves and the tumor: surgically by cutting the gastric vagus nerve (vagotomy), by local injection of Botox to block the release of neurotransmitter from the vagus nerve, by giving a drug to block the receptor of the neurotransmitter, and by knocking out of the receptor gene. All procedures suppressed the tumor growth.
"But we found that the anti-cancer effects were remarkable, especially with local vagotomy or by injecting Botox. It actually surprised us. The finding that Botox was highly effective was particularly exciting," Chen said.
Botox is well known to the public as a beauty treatment, but it is also used for different medical indications.
"We believe this treatment is a good treatment because it can be used locally and it targets the cancer stem cells. The Botox can be injected through gastroscopy and it only requires the patient to stay in the hospital for a few hours," says Chen.
He added that the procedure is also less toxic than most standard cancer treatments, less expensive and has hardly any side effects.
"However, for most patients, we are suggesting that denervation works best in combination with traditional chemotherapy, since loss of nervous input appears to make cancer cells more vulnerable to chemotherapy, which makes the chemotherapy more efficient as well," Wang said.
The promising results from this study have led to an initiation of a phase II clinical trial for patients with stomach cancer in Norway.
The Botox treatment can be an additional treatment for patients who have inoperable stomach cancer, or patients who have received chemotherapy but no longer respond to such therapy. It can also be considered in patients who, due to toxicity of chemotherapy, cannot be offered chemotherapy treatment or who, after meticulous information about chemotherapy, still do not want such treatment.
"The nerve-tumor growth connection is likely to be true in other solid tumors, such as in prostate cancer, but the precise nerves that are involved are likely to vary from organ to organ and tumor to tumor. Further studies are needed," both Chen and Wang added.