Beta-catenin alters T cells in lasting and harmful ways
Study helps explain chronic inflammation in autoimmunity and cancer
Advertisement
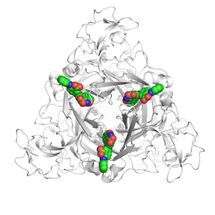
Activation of beta-catenin, the primary mediator of the ubiquitous Wnt signaling pathway, alters the immune system in lasting and harmful ways, a team of Chicago-based researchers demonstrate in the issue of Science Translational Medicine.
An increase in beta-catenin in certain types of T cells—a class of white blood cells—causes chronic inflammation in the intestine and colon, eventually leading to cancer. The same mechanism is used by colon cancer to propagate itself. The researchers combine data from patients suffering from colitis or colon cancer with studies in mouse models of the disease to unravel the mechanism of this transition.
"We initially focused on this process in mouse models of hereditary colon cancer (polyposis), but the breakthrough came when we went to see patients," said the study's principal investigator, Fotini Gounari, PhD, associate professor of medicine at the Gwen Knapp Center for Lupus and Immunology Research at the University of Chicago. "Biopsied tissues from colitis patients contained T cells with high levels of beta-catenin. When we examined blood from colon-cancer patients, we found the same pathway activated in both conventional T cells and regulatory T cells."
Previous work by the team showed that a subset of protective T cells known as regulatory T cells, or Tregs—which normally stifle inflammation—switches functions in colon cancer patients to promote inflammation and enhance tumor growth.
The current study points to beta-catenin as the primary culprit. The researchers found mounting levels of this protein in T cells from patients with long-lasting ulcerative colitis and colon cancer. When Gounari and colleagues genetically engineered mice so that their T cells expressed high levels of beta-catenin, those mice were highly susceptible to colon cancer.
The finding "was a revelation," Gounari said. Activation of this signaling pathway appears to be an initiating event for colon cancer, which is then fed by uncontrolled inflammation in the tumor environment.
Normally, inflammation in the gut is elevated through the action of T-helper 17 (TH17) cells and suppressed by Tregs. This balance is important for keeping microbes in the gut at bay and for stimulating growth of cells during tissue repair. However, in colon cancer, a distinct set of regulatory T cells that have pro-inflammatory properties, expands rapidly and upsets the balance.
"We now have evidence that beta-catenin is a key molecule for expansion of both TH17 cells and pro-inflammatory Tregs," Gounari said.
With their unique mouse models, Gounari and colleagues were able to tease apart some of the mechanisms that generated pro-inflammatory T cells. They found that beta-catenin signaling initiated a cascade of events in both conventional T cells and Tregs that altered the chromatin organization and the type of genes expressed by T cells. These changes activate a protein called RORγT that was previously known to direct the differentiation of TH17 cells.
"It's like a tsunami," said collaborating partner, Khashayarsha Khazaie, PhD, professor of immunology at the Mayo Clinic. "If you make both your conventional T cells and Tregs pro-inflammatory, then you've done it. You've lost control in a bad way."
Understanding the process will provide ways to intervene in many diseases, the authors suggest.
"We want to disrupt the signals," Gounari said. "There are inhibitors under development that block RORγt or selectively interrupt the Wnt pathway in T cells. If you could block the pathway enough to tip the balance back to normal, that could potentially stop inflammatory bowel diseases and help control colon cancer."
"Activation of beta-catenin in T cells is unlikely to be restricted to these diseases, and is likely to happen in other autoimmune diseases and cancers, so there may be broad prospects for therapy of a range of chronic and often lethal diseases," she adds.
There is still work to be done, the researchers emphasize. They hope to learn more about how beta-catenin produces chromatin changes that disturb normal immune function, how this system interacts with the microbiome, and to determine the best targets for therapy.
But they have taken an important step. "Elucidating the molecular mechanisms that shift the lymphocyte balance from anti-inflammatory to proinflammatory," they wrote, "is expected to improve diagnosis and treatment of autoimmune diseases and cancer."