Study outlines risk factors for poor outcome, mortality following hip fracture
Commencing surgery sooner may alleviate hip fracture complications
A new study identifies predictors of complications and mortality following a hip fracture, including dialysis, cardiac disease, diabetes, and a longer time before surgery – the only modifiable risk factor when patients are hospitalized.
Each year, more than 340,000 Americans are hospitalized for hip fractures. According to AAOS data, 69 percent of hip fracture patients are female and 46 percent are between the ages of 65 and 84. Many hip fracture patients suffer complications with life-altering consequences. The estimated mortality rate within one year of a hip fracture ranges from 12 to 33 percent.
In the study, researchers used data from the 2008 National Sample Program (NSP) of the National Trauma Data Bank (NTBD) to identify a representative sample of 44,419 hip fractures. Among the specifics:
- The average patient age was age 72.7.
- Sixty-two percent of patients were female.
- Patient demographics, medical comorbidities, injury-specific factors and outcomes were recorded and a national estimate model developed for analysis.
Primary outcomes included mortality and the development of complications (4.5 percent and 12.5 percent, respectively). Seventeen percent of patients who sustained at least one complication died. Secondary measures consisted of the development of specific complications such as pulmonary/cardiac complications, venous thromboembolic disease and infection.
Hypertension and diabetes were the most common medical comorbidities among patients. Dialysis, presenting in shock, cardiac disease, male sex and a high Injury Severity Score (ISS) were significant predictors of mortality. Dialysis, shock, obesity, cardiac disease, diabetes and a greater time to surgery significantly influenced the risk of developing one or more post-operative complications. Obesity, femoral neck (the uppermost section of the thigh bone) fracture, cardiac disease and diabetes significantly increased the risk of developing major complications. The presence of shock following injury was the most important predictor of both cardiac and venous thromboembolic disease complications with an odds ratio exceeding 10 for the development of cardiac complications.
"Most of the predictors of complications and mortality are non-modifiable," including the presence of significant cardiac/respiratory disease, diabetes, dependence on dialysis and presentation to the hospital in shock, said Philip J. Belmont, Jr., MD, an orthopaedic surgeon at the William Beaumont Army Medical Center in El Paso, Texas, and the lead author of the study.
"Reduced time to surgical intervention appears to be the single greatest factor with which a surgeon might influence the risk of mortality or complications," said Dr. Belmont. A previous study has shown a 41 percent increase in mortality if surgery is delayed 48 hours or more. The majority of patients are taken into surgery within 24 hours.
In older hip fracture patients, the pre-operative "work-up," and/or the correction of major clinical abnormalities – important and frequent considerations – can sometimes take more than one day, said Dr. Belmont. The potential benefit of correcting major clinical abnormalities prior to hip fracture surgery can influence survival. This process often can be expedited when the orthopaedic surgeon works directly with the internal medicine physician or hospitalist who is helping to manage the patient.
"With the rising incidence of hip fractures, patient-treatment solutions directed toward this modifiable factor may reduce complications, and potentially, mortality," said Dr. Belmont.
Most read news
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents

Mobile phone use may affect semen quality - Is 4G less harmful than 2G?
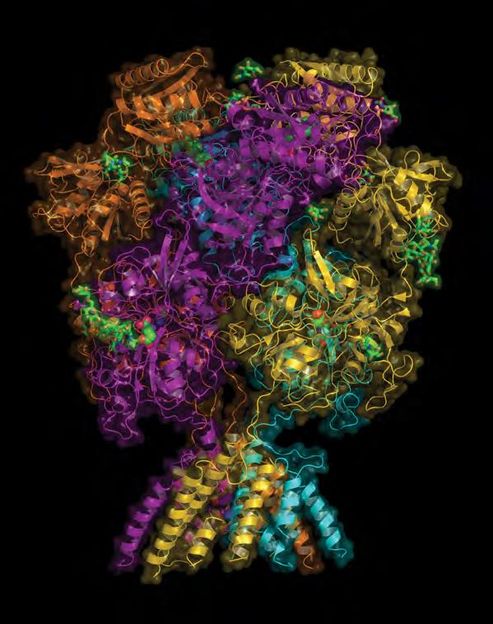
New theorem helps reveal tuberculosis' secret

FLAM-seq: the full picture of messenger RNA and their tails
Alligator Bioscience to Receive USD 6 Million Milestone Payment from Janssen
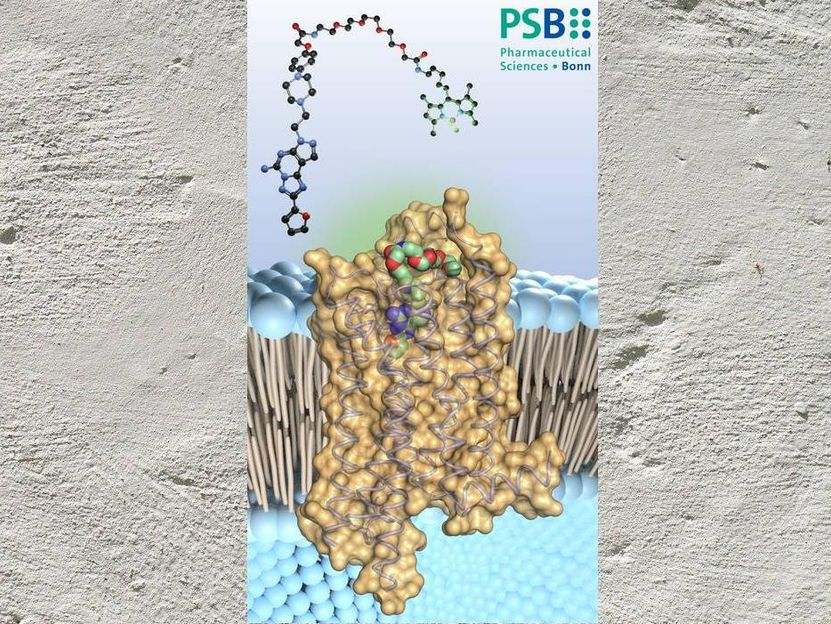
Study shows how bioactive substance inhibits important receptor - Results from the University of Bonn raise hope for new drugs against cancer and brain diseases
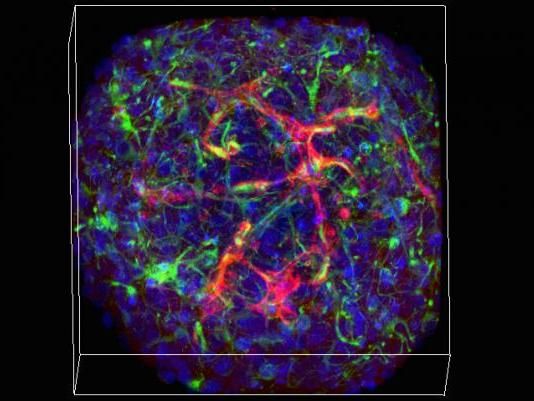
With mini-vessels, mini-brains expand research potential

Scientists engineer new potent antibiotic - Darobactin 22 could have the potential to become the next antibiotic superstar
How biofuels from plant fibers could combat global warming

DNA Chips as Storage Media of the Future
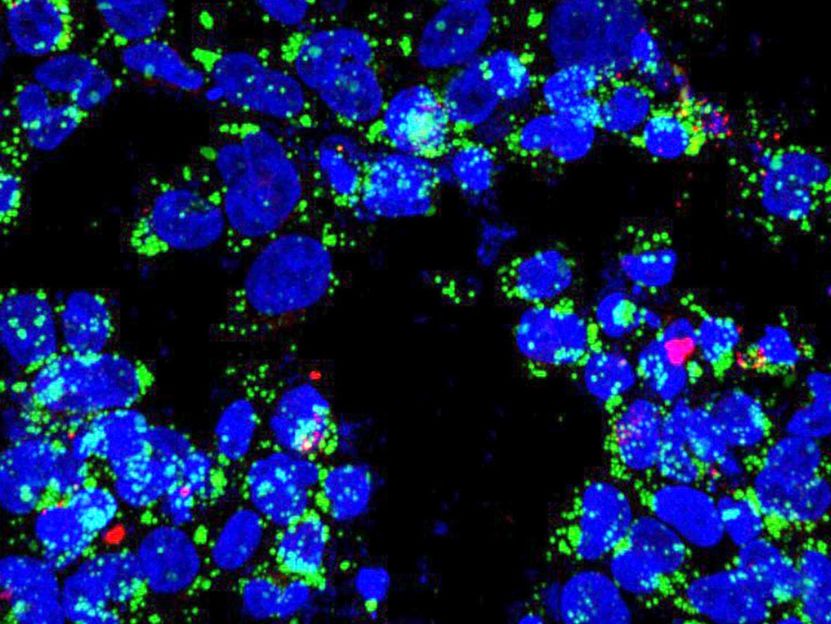
Tiny “blinkers” reveal molecules inside cells

BASF lifts force majeure for key vitamin A and E products