Temple scientists target DNA repair to eradicate leukemia stem cells
Despite treatment with imatinib, a drug that targets chronic myeloid leukemia (CML, some patients may continue to be at risk for relapse because a tiny pool of stem cells is resistant to treatment and may even accumulate additional genetic aberrations, eventually leading to disease progression and relapse. These leukemia stem cells are full of genetic errors, loaded with potentially lethal breaks in DNA, and are in a state of constant self-repair.
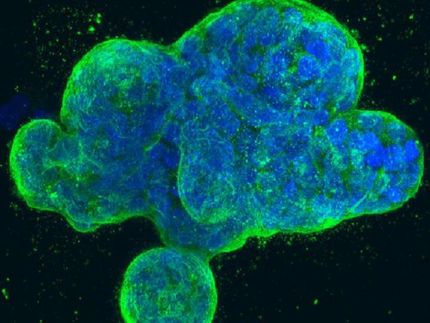
Now, scientists at Temple University School of Medicine may have figured out a way to corral this stem cell activity and stunt further cancer development. In a series of experiments in mice with cancer and in cancer cells, they have shown that they can block the process by which leukemia stem cells repair themselves by targeting a particular protein, RAD52, which the cells depend on to fix genetic mistakes. The findings may lead to a new strategy to help overcome drug resistance that hinges on cancer stem cells gone awry.
"We would like to eradicate the leukemia stem cells and cure patients with CML," said senior author Tomasz Skorski, MD, PhD, Professor of Microbiology and Immunology at Temple University School of Medicine. "We took advantage of the fact that remaining leukemia stem cells accumulate lots of lethal DNA lesions, but they don't die because they can repair them very efficiently. We attacked the DNA repair pathway in a way that is not going to harm normal cells, which have a different repair mechanism than leukemia cells."
Targeting Key Repair Protein
The trick, the researchers say, lies in a process called "synthetic lethality," which is defined as a genetic combination of mutations in two or more genes that leads to cell death, whereas a mutation in any single gene does not. In synthetic lethality, cancer cells may accumulate mutations fostering their growth, enabling them to sidestep certain types of anticancer treatments. But these same genetic mutations may make them vulnerable to a different type of therapy.
In CML, an enzyme called ABL1 goes into overdrive because of a chromosomal mix-up that occurs in bone marrow stem cells that are responsible for the generation of all blood components. The genes ABL1 and BCR become fused and produce a hybrid BCR-ABL1 enzyme that is always turned on. This overactive BCR-ABL1 protein drives the excessive production of white blood cells that is the hallmark of CML.
CML is also marked by genomic instability, which can result in mutations that cause the cancer to become resistant to potent targeted anticancer drugs called tyrosine kinase inhibitors (TKIs), such as imatinib (Gleevec), leading to disease relapse and perhaps to the deadlier blast stage of the disease. One of the most common types of DNA damage is a "double-strand break," which entails severing both of the complementary strands of DNA that make up the double helix.
In CML cells, the BCR-ABL1 protein shuts down the main DNA repair system and leukemia cells have to rely on a backup pathway for repair. Previous experiments in mice bone marrow cells lacking RAD52, a key protein in the backup system, showed that its absence abrogated the development of CML, proving that CML DNA repair depended on RAD52.
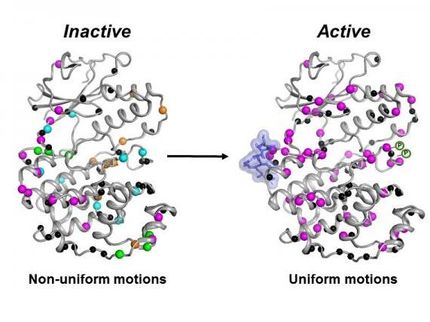
"Earlier research by Temple investigators found that the presence of the RAD52 gene is a key factor for the development of the leukemia," explained first author Kimberly Cramer, PhD, a postdoctoral fellow in the Department of Microbiology and Immunology at Temple's School of Medicine. The researchers took advantage of the fact that when the RAD52 protein is mutated in some way, it can no longer bind to DNA, which is crucial to fixing broken DNA. Using the same bone marrow cells that lacked RAD52, they re-expressed either normal RAD52 or, more importantly, either of two mutated forms of RAD52 to see what would happen when RAD52 could not bind to DNA anymore.
They found that when the mutant RAD52 proteins were expressed in the presence of BCR-ABL1, there were more double-strand breaks formed, which was accompanied by a decrease in the survival and expansion of leukemia stem cells. The team then used an "aptamer," a peptide that mimicked the area where the RAD52 protein binds to DNA, to see the effects of blocking RAD52 from binding to DNA. The investigators found that when the aptamer was added to BCR-ABL1-positive bone marrow cells, RAD52 was prevented from binding to DNA and the leukemic bone marrow cells accumulated excessive double-strand breaks and eventually died. The aptamer had no effect on normal cells.