Blocking key protein could halt age-related decline in immune system, Stanford study finds
The older we get, the weaker our immune systems tend to become, leaving us vulnerable to infectious diseases and cancer and eroding our ability to benefit from vaccination. Now Stanford University School of Medicine scientists have found that blocking the action of a single protein whose levels in our immune cells creep steadily upward with age can restore those cells' response to a vaccine.
This discovery holds important long-term therapeutic ramifications, said Jorg Goronzy, MD, PhD, professor of rheumatology and immunology and the senior author of a study to be published online Sept. 30 in Nature Medicine. It might someday be possible, he said, to pharmacologically counter aging's effects on our immune systems.
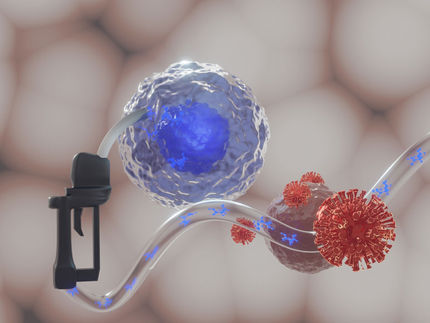
In the study, the Stanford team fingered a protein called DUSP6 that interferes with the capacity of an important class of immune cells to respond to the presence of a foreign substance, such as those appearing on the surface of an invading pathogen or in a vaccine designed to stifle that invasion.
The researchers also identified a potential lead compound that, by inhibiting DUSP6's action, restores those cells' responsiveness to a more youthful state.
A person's immune response declines slowly but surely starting at around age 40, said Goronzy. "While 90 percent of young adults respond to most vaccines, after age 60 that response rate is down to around 40-45 percent. With some vaccines, it's as low as 20 percent." Vaccine failure among seniors poses a serious health problem: Some 90 percent of influenza deaths are among people over age 65.
A vaccine is, in essence, a "mug shot" of one or more of a pathogen's most prominent features, akin to a photo of a giant wart on a suspect's nose. This chemical snapshot — or antigen, in scientific parlance — is nailed into customized "frames" and displayed on the surface of "desk cop" cells specializing in signaling T cells, the "beat cops" of the immune system.
One important type of beat cop, the so-called T-helper cell, stimulates other immune cells called B cells that play a key role in our response to infection-preventing vaccines. On exposure to an antigen from a vaccine or the pathogen itself, along with appropriate interactions with T-helper cells, B cells proliferate, mature and get down to brass tacks: producing and secreting antibodies. These molecules are designed to snare and immobilize the pathogen, flagging it for incarceration and, quite likely, a death sentence meted out by still other very tough immune cells.
For poor responders, there are a few ways of increasing a vaccine's potency. One is to simply boost the dose. A second is the use of adjuvants: chemicals, or combinations of them that, like a cup of strong coffee, wake up the desk cops whose job is to display the description of the pathogen's distinguishing feature (the antigen) to the beat cops. A recently published large, multicenter study, one of whose co-authors was Cornelia Dekker, MD, professor of pediatrics (infectious disease) at Stanford, showed that adding an experimental adjuvant to the standard seasonal flu vaccine substantially improved seniors' response to the vaccine.
But just waking up the desk cops won't cut it if the beat cops are too sluggish. Older people's T-helper cells suffer from a diminished capacity to activate, proliferate and secrete crucial signaling chemicals in response to infections or vaccines. This limits even an adjuvant-containing vaccine's ability to get the job done.
"Some age-associated defect or defects raise the threshold of responsiveness to the presented antigen, so a vaccine dose that triggers T-cell activation in a younger person doesn't in an older person. Adjuvants can't compensate for these defects," Goronzy said.
So he and his team sought to identify the defects that cause this age-related sluggishness in T-helper cells, and to see how to counter them.
Circulating T-helper cells fall into two broad categories. "Naïve" T-helper cells have never encountered an antigen before (as in the case of, say, a rare or emerging pathogen or a new vaccine), but are capable of wheeling into action once they do. It takes a week or two to reach full tilt.
"Memory" T-helper cells have previously been exposed to an antigen. These cells are long-lived and narrowly fixed on that particular antigen. They can rapidly transition to an activated state should the same antigen ever cross their path again. That's why prior exposure — through infection or a vaccine — renders us more resistant.
In a Proceedings of the National Academy of Sciences study published earlier this year, Goronzy's team showed that faulty regulation in memory T-helper cells, due to aging-related increased levels of a protein called DUSP4, inhibits the activation of those cells, with their consequent failure to ignite a good B-cell (antibody-producing) response.
This time around, the investigators uncovered a similar effect with a related protein, DUSP6, on naïve T-helper cells. In test tubes, they compared blood cells drawn from people ages 20-35 versus 70-85 in response to stimulation. In naïve T-helper cells (but not in memory cells), there were age-associated differences in a specific chain of biochemical events involved in the cells' activation, proliferation and differentiation. Laboratory tests showed that the culprit behind the cells' fecklessness in older people was DUSP6, an enzyme that works by hacking phosphate groups off of other enzymes, thus dialing down their activity. Those "downstream" enzymes are crucial to naïve T-helper cell activation. DUSP6 levels were much higher in older people's naïve T-helper cells.
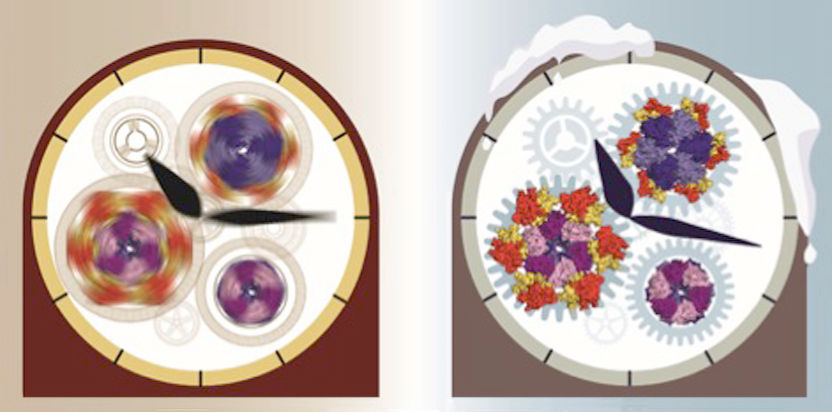
Further experimentation revealed that DUSP6's increase in aging naïve T-helper cells was caused by an age-associated easing up on a brake pedal called miR-181a, one among hundreds of small molecules made of RNA (called microRNA) that regulate proteins' production. All microRNA molecules work by affixing themselves to larger protein-template RNA molecules, also made of RNA, gumming things up and stalling the procedure. Each distinct variant of microRNA molecule can bind to several different varieties of protein-prescribing RNA molecule, thereby swiftly redirecting a cell's overall behavior.
Goronzy and his colleagues saw that miR-181a directly interferes with the production of DUSP6 and noted that the amount of miRNA-181 present in naïve T-cells declines steadily, bottoming out around age 65-70, causing levels of DUSP6 in these cells to increase with age. Artificially boosting miRNA-181a levels in naïve human T cells caused DUSP6 levels to plummet, commensurately increasing those cells' readiness to activate on exposure to a given dose of influenza vaccine. In contrast, artificially increasing the levels of DUSP6 blocked the beneficial effects of heightened miR-181a levels.