How malnutrition leads to inflamed intestines
Researchers at the Institute of Molecular Biotechnology in Vienna, Austria, have uncovered how malnutrition, affecting millions of people, leads to diarrhoea, inflamed intestines and immune system disorders. This surprising result explains food effects that have been known for centuries and provides a molecular link between malnutrition and the bacteria which live in our intestines.
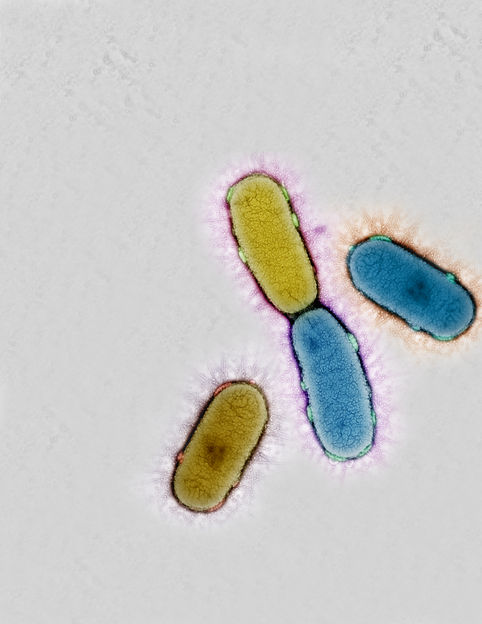
Intestinal bacteria
IMBA/CSF EM
More than one billion people in poor countries are starving, and malnutrition remains a major problem even in rich countries, making it a leading cause of death in the world. For over a hundred years, doctors have known that a lack of protein in the diet or low levels of amino acids, the building blocks of proteins, can lead to symptoms like diarrhoea, inflamed intestines and other immune system disorders, which weaken the body and can be fatal. However, the molecular mechanism which explains how malnutrition causes such severe symptoms has been largely unexplored.
Now a research group led by Josef Penninger, the director of the Institute of Molecular Biotechnology (IMBA) in Vienna, Austria, in cooperation with Philip Rosenstiel, University of Kiel, Germany, has found a molecular explanation for the increased susceptibility to intestinal inflammation in malnutrition. The researchers were studying an enzyme which helps to control blood pressure, kidney failure in diabetes, heart failure and lung injury, called the Angiotensin Converting Enzyme 2, or ACE2. This enzyme was identified as the key receptor for SARS virus infections, but the researchers also discovered an entirely new function. ACE2 controls the way our intestines take in amino acids from our food, via amino acid transporters, and in particular the uptake of the essential amino acid tryptophan.
Too little tryptophan alters our natural immune system, which changes the types of bacteria which can live in our bowels and guts, leading to higher sensitivity and eventually diarrhoea and inflamed intestines. Increasing the intake of tryptophan in their diet provided relief for mice suffering from intestinal inflammation. The mixture of bacteria returned to normal, the inflammation died down, and the mice also became less susceptible to new attacks.
"The research shows how the food we eat can directly change the good bacteria in our intestines to bad bacteria and so influence our health”, says Thomas Perlot, the first author of the study. “Our results might also explain nutritional effects that have been known for centuries and provide a molecular link between malnutrition and the bacteria living in our intestines. This discovery could be used in the future to treat patients with a simple regulated diet or by taking tryptophan as a food supplement. And there is hardly any risk of side effects from artificially increasing an amino acid found in the normal diet.”
Josef Penninger, the lead author, says “I have studied ACE2 for more than 10 years and was completely stunned by this novel link between ACE2 and amino acid balance in the gut. Biology continues to surprise me. Up to a billion people in the world are malnourished, especially the poor and disadvantaged. In Austria alone, around 80,000 people suffer from a chronic inflammatory bowel disease like ulcerative colitis or Crohn's disease. I hope that our findings have opened a door to a better molecular understanding how malnutrition affects human health. Whether simple tryptophan diets can indeed cure the effects of malnutrition in humans now needs to be carefully tested in clinical trials.”
Original publication
„ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation“; Nature
Original publication
„ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation“; Nature
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
More news from our other portals
Last viewed contents
Genentech to set up Singapore's first Microbial-Based Biopharmaceutical Manufacturing Facility - Fourth Biologics Facility in Less Than 2 Years Helps Establish Singapore as a Serious Player in Biologics Manufacturing
Arakis completes Phase I trials of AD 337 in fibromyalgia syndrome
ABRAXANE meets primary endpoint in phase 3 trial for advanced non-small cell lung cancer
Oncolytics Biotech Inc. has been granted patent for extracting virus from cell culture
Researchers identify genes linked to chemoresistance





















































