How metastasizing cancer cells enter organs
It is not primary tumors that are responsible for the majority of cancer deaths, but rather their metastases. Physiologists and neuropathologists from the University of Zurich have now identified the origin of metastasis formation, thereby becoming the first to reveal the pathway of metastasizing intestinal cancer cells out of the blood stream. The results allow new approaches in the development of cancer therapies.
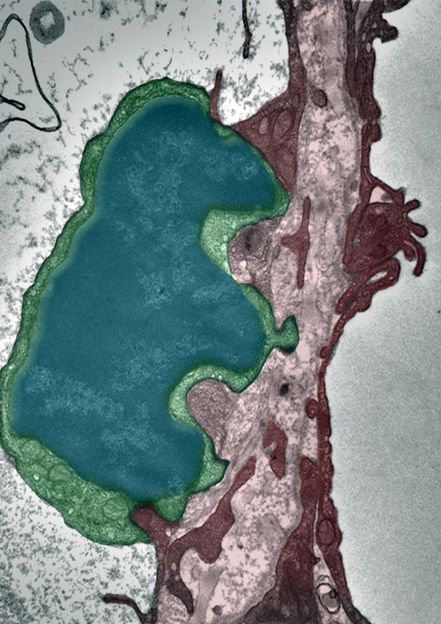
Electron microscopy from a tumor cell that is on the way to extravasate through an alveolar endothelium blood capillaries – the tumor cell is depicted in blue green, the endothelial cell in purple red. The protrusion of the tumor cell are seen that form their way through the endothelial cell.
UZH
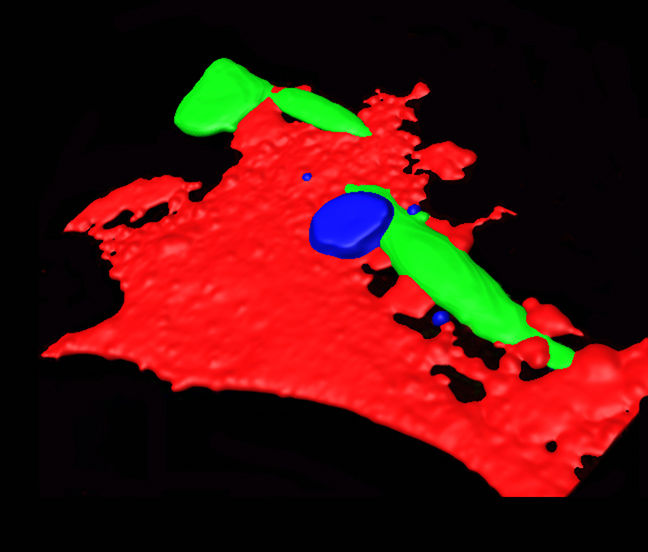
Tumor cells (green) adhere on the endothelium (red) that gets activated and permeable through CCL2-CCR2 signaling. Tumor cell extravasation is facilitated by recruited monocytic cells (blue). Technique: Adaptation of confocal image stacks creating an artificial surface.
UZH

Every year, over seven million people die of cancer worldwide. Thanks to more effective therapy and better early detection, primary tumors are only responsible for ten percent of cancer deaths in industrial nations. Nowadays, the vast majority die from the consequences of metastasis, namely secondary tumors. These develop from metastases of the primary tumor by spreading via the patient’s bloodstream. Until now, the actual reason for the metastatic spread in certain organs was unknown, it being unclear as to how the secondary cells were able to enter the tissue of other organs from the bloodstream.
Now, a European team headed by physiologists and neuropathologists from the University of Zurich have identified the mechanism that helps metastasizing intestinal cancer cells to infiltrate the organs from the blood vessels. Lubor Borsig and Mathias Heikenwalder’s team demonstrate that cancer cells manipulate specific “doorman receptors” on the endothelium of the blood vessels.
Tumor cells manipulate blood-vessel doorman
Chemokines (intercellular messengers) play a key role in the immune system: They can summon white blood cells directly for immune defense. Tumor cells are also capable of producing chemokines and mobilizing the body’s own special immune cells, monocytes. Consequently, elevated levels of the tumor’s own chemokine CCL2 are characteristic of metastasizing breast, prostate and bowel cancer. Until now, high CCL2 values were primarily taken as an indication of strong tumor growth and a poor prognosis for the disease. Based on in-vivo and in-vitro experiments on lab mice, Borsig and Heikenwälder show that CCL2 is far more than an indicator of the cancer’s aggressiveness. “CCL2 activates a doorman receptor and enables cancer cell to leave the blood circulation and metastasize in other organs,” explains Borsig. The role of the doorman detected on the endothelium for the first time and referred to as CCR2 in a healthy organism is not known. Borsig suspects that the doorman modulates the permeability of the blood vessels during the body’s immune response.
New approach for drug development
“The mechanism discovered will yield a completely new approach for the development of drugs to combat metastasis in breast, prostate and bowel cancer,” Borsig is convinced. Suppressing the tumor’s chemokine expression or blocking the doorman for the tumor chemokine to inhibit any more cancer cells from entering healthy tissue from the bloodstream is conceivable. “If we can succeed in preventing the cancer cells from leaving the bloodstream, the metastasis can be fought directly at the source,” concludes Borsig.



















































