Anti-inflammatory drugs may improve survival from severe malaria
A novel anti-inflammatory drug could help to improve survival in the most severe cases of malaria by preventing the immune system from causing irrevocable brain and tissue damage.
Walter and Eliza Hall Institute researchers have shown that a new class of anti-inflammatory agents, called IDR (innate defense regulator) peptides, could help to increase survival from severe clinical malaria when used in combination with antimalarial drugs.
A research team fronted by Dr Ariel Achtman and Dr Sandra Pilat-Carotta, and led by Professor Louis Schofield from the institute's Infection and Immunity division, published the study today in the journal Science Translational Medicine.
Dr Achtman said that many drugs that prevent malaria infections are not effective in sick patients at preventing tissue damage that arises from the inflammatory immune response. "The most severe forms of malaria, such as cerebral malaria which causes brain damage, are actually the result of the immune system trying to fight infection and causing collateral damage," she said.
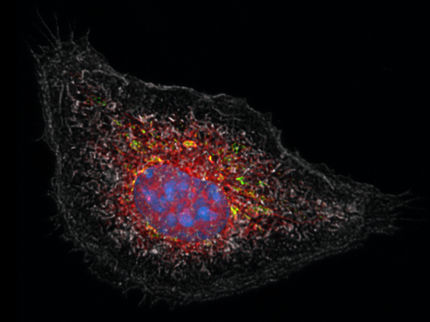
Dr Pilat-Carotta said the team used a treatment approach combining drugs that suppress potentially harmful inflammation with antimalarial agents that fight the parasite, in mouse models infected with the malaria parasite Plasmodium berghei. "In this study, we showed that a new class of drugs could prevent inflammation in the brains of mice with malaria and improve their survival. This is an example of a 'host-directed' therapy – a treatment intended to act on the host not the parasite," Dr Pilat-Carotta said.
Professor Schofield said up to 25 per cent of severe clinical malaria cases are fatal even with access to the best health care. "Antimalarial drugs are very effective, but only if they are given before serious clinical symptoms develop. On their own, antimalarial drugs fail in approximately one out of every four cases of severe clinical malaria, because by the time the patient arrives at a hospital they are already very sick and inflammation caused by the immune response to the parasite is causing major organ damage," Professor Schofield said.
IDR peptides are a new class of anti-inflammatory agent developed by Professor Robert Hancock and colleagues at the University of British Columbia, Canada, which enhance beneficial aspects of the initial immune response, while dampening harmful inflammation, Professor Schofield said. "IDR peptides are also relatively cheap to produce and easy to use, making them a good option for medical treatments in developing countries," he said.
Dr Achtman said the development of preclinical models of severe malaria could improve pre-clinical drug screening and potentially prevent some of the drug failures that happen at the human clinical trial stage. "Professor Gordon Smyth and Ms Charity Law from the institute's Bioinformatics division used sophisticated bioinformatics-driven analyses to identify early changes to inflammatory processes, days before the mice show visible changes in malaria disease symptoms. Host-directed therapies are a good treatment option because parasites are less likely to evolve resistance, and we believe they will eventually increase the number of successful treatment interventions in the short time window between hospitalisation with severe malaria and death," Dr Achtman said.
Most read news
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.