Dual strategy to fight Type 1 diabetes
Advertisement
University of Florida researchers teamed with colleagues at City of Hope National Medical Center in Duarte, Calif., to devise a new combination therapy that reverses established type 1 diabetes in mice.
The findings, which appear in Science Translational Medicine, set the stage for the development of a new human therapy for Type 1 diabetes that is effective over the long term.
The two-step regimen involves bone marrow transplantation and substances that promote the growth of cells that produce insulin, the sugar-regulating hormone that is missing in people who have Type 1 diabetes.
“If our therapy is successfully translated to humans, patients will be able to have a life without Type 1 diabetes — that’s the exciting part,” said senior author and UF collaborator Defu Zeng, M.D., an associate professor of hematology and hematopoietic cell transplantation at City of Hope.
UF Type 1 diabetes experts Brian Wilson, M.D., Ph.D., and Mark Atkinson, Ph.D., professors in the College of Medicine department of pathology, immunology and laboratory medicine and the UF Diabetes Center of Excellence, are key members of the research team, which also demonstrated that insulin-producing cells can come from other types of cells altogether.
Type 1 diabetes arises when the body’s immune system attacks cells in the pancreas that produce insulin, whose job is to move sugar out of the blood so it can be converted to energy. As a result, glucose builds up in the blood, causing organ damage. More than 1 million people in the United States live with Type 1 diabetes, according to the Centers for Disease Control and Prevention. And more than 30,000 new cases are diagnosed each year. People who have the disease must take insulin injections to survive, but insulin supplementation does not cure Type 1 diabetes nor prevent complications such as blindness, kidney disease and heart disease.
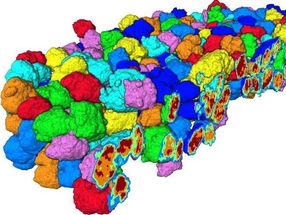
The only existing therapy that can reverse established Type 1 diabetes is transplantation of a type of pancreatic tissue called islets, which contain the insulin-producing beta cells. But chronic rejection is a big problem with that approach, and the diabetes-reversing effect lasts only about three years. In addition, to get enough cells for each patient, two or three donors have to be found.
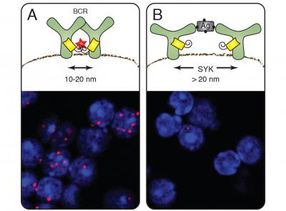
Researchers have continued to explore various ways to counteract the body’s attack on insulin-producing cells. They have developed methods to blunt the action of immune system cells against beta cells. And previous experiments have shown that in the early stages of Type 1 diabetes, some insulin-producing cells still exist and can be cajoled into action. But at advanced stages of disease, those cells are mostly destroyed.
The researchers concluded that a dual approach that prevents the immune system from killing beta cells, and, at the same time, replenishes the supply of beta cells was needed.
They used a growth hormone and another chemical to stimulate the production of new beta cells. In so doing, they verified that the treatment could induce new insulin-producing cells in mice whose immune system is programmed to kill those cells. And it turned out that the new cells came not just from the replication of existing cells, but also from the transformation of other kinds of cells.
“It’s conceptually a new way to go after Type 1 diabetes treatment, and lends strong support to the idea that beta cells can — and do — come from a source that is not beta cells undergoing replication,” Wilson said.
The findings suggest that, given the right stimulation, patients with diabetes could produce the needed cells on their own instead of having to wait for transplants from donors.
But by itself, generation of new beta cells was ineffective at reversing late-stage Type 1 diabetes in the mouse models, because the immune system kills those cells as soon as they appear. First, the researchers had to create a safe environment that would allow the new cells to survive. For that, they explored an option more commonly thought of as a treatment for leukemia. Bone marrow transplantation has been shown to help the immune system learn how to recognize and tolerate newly formed insulin-producing cells. Together, the therapies did the trick, reversing late-stage diabetes in 60 percent of the mice in the study.
“This gives a mechanism where you could use this bone marrow engraftment combined with growth factors to reverse established diabetes — that, I think, is the really big thing there,” said David Serreze, Ph.D., a professor at The Jackson Laboratory in Bar Harbor, Maine, and an adjunct associate professor at the University of Massachusetts Medical School, who was not involved in the current study. “The individual components had been known before, but it was a very ingenious way of pulling them all together.”
The UF collaborators and Zeng are working to form a national collaboration to further investigate and develop the new combination therapy.
“This is not going to be in the clinic tomorrow,” Serreze said. “But is this something you could envision being used sometime in the future? Oh, absolutely.”