Antimicrobial-resistant bacteria in the stable - what risk does it pose to humans?
Measures to combat resistance must focus on both, clinics and stables
Not only in hospitals but also in production animals, the resistance of bacteria to antimicrobials is on the increase. Resistant strains are found in both pathogenic germs, and in non-pathogenic bacteria or so-called commensal bacteria. This development is not surprising. After all, every time antimicrobials are used, this results in selective pressure, and bacterial strains which have developed defence mechanisms against the used antibiotic can spread. This applies to both animal stables and hospitals. Detection of resistant germs is nothing new: antimicrobial-resistant bacteria have been found in both production animals (poultry, pigs, and cattle) and on food samples (pork, poultry meat and raw milk). "Both in the clinic and in production animals, the use of antimicrobials must be restricted to what is indispensable from a therapeutic viewpoint", says th e President of the Institute for Risk Assessment Dr. Dr. Andreas Hensel. "In the area of production animals, we must ensure that the animals are healthier overall and that wherever possible they do not need treatment with antimicrobials in the first place. This must be achieved by breeding more robust animals and through improved housing conditions which include profound prophylactic vaccination, better hygiene, and good stable management." An investigation from North Rhine-Westphalia shows that no general connection is obvious between treatment intensity and size of enterprise.
The use of antimicrobials does not result principally in the development of new antimicrobial resistance in bacteria. Rather, bacteria that have become resistant, typically by accident through mutation, have an advantage over non-resistant strains when antimicrobials are used. In consequence, such bacteria then multiply more quickly than non-resistant germs.
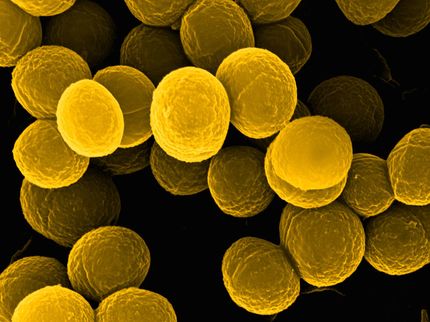
Thanks to resistance monitoring, the Federal Institute for Risk Assessment has been aware for quite some time that zoonotic pathogens such as salmonella and campylobacter which show resistance to modern antimicrobials such as fluoroquinolones and cephalosporins are present in production animals and in food derived from them such as meat. These types of antimicrobials should be used with caution in the treatment of production animals. Additionally, studies of poultry, pig and cattle stocks show that the incidence of methicillin-resistant staphylococcus aureus (MRSA) and ESBL-carrying bacteria has increased over the last few years. However, the MRSA detected in production animals only account for a very small proportion of cases of illness in humans. The vast majority of those affected are persons who have regular contact with production animals through their profession. MRSA infections contracted in hospitals are almost exclusively strains which a re only found in humans. To what extent infections with ESBL-producing bacteria in humans originate from animal production is currently the subject of research. So far, no direct evidence for a direct infection chain exists. Nevertheless, molecular studies suggest that ESBL-producing bacteria from animal production do pose a risk to human health. For this reason, a situation must be prevented where the antimicrobial-resistant germs from animal stables become a problem for humans via food or through contact with animals.
In line with this insight, the German antimicrobial resistance strategy (DART) was launched based on close cooperation between the Federal Ministry of Health, the Federal Ministry of Nutrition, Agriculture and Consumer Protection as well as the Federal Ministry of Education and Research as early as 2008. Consisting of a package of measures taken both in human medicine and in animal production, the campaign aims to curb resistance to antimicrobials. For this purpose, data on the antimicrobial resistance situation and development for bacterial pathogens are collected both in human and veterinary medicine. These results should enable physicians and veterinarians to choose the correct substances and use them in the most efficient manner possible in cases where treatment of humans or animals becomes necessary. In the area of animal keeping and food production, the principal goal is to preserve or enhance the health of the animals through preventive measures, so that infections of production animals are avoided. Among other things, this includes consistent control of zoonotic pathogens in livestock, good hygiene in the stable, good animal care and systematic vaccination programmes. Through enhanced animal health, the administration of antimicrobials for the treatment of illness can be minimised. At the same time, better recording procedures of the use of antimicrobials in veterinary medicine aim to simplify control of the use of such drugs.
In the opinion of the Federal Institute for Risk Assessment, the risk of contracting, via food, an untreatable infection from antimicrobial-resistant pathogens is currently low for consumers, provided that the rules of kitchen hygiene are observed. On the basis of a common effort made by the authorities, veterinarians, and animal production businesses, this as yet favourable situation should at the very least be preserved at all costs.