UF researchers suspect bacterial changes in mouth promote oral disease in people with HIV
Oral disease occurs commonly and progresses rapidly among people who have HIV, but the process is poorly understood. Researchers suspect that the culprit is a change in the makeup of bacterial communities that live in the mouth.
Through a one-year grant of almost $330,000 from the National Institutes of Health, researchers at the University of Florida are trying to find out the role of various pathogens in the progression of oral disease among people infected with HIV.
“The hypothesis is that suppression of the immune system by HIV contributes to changes in the oral biota, which then contributes to oral disease,” said Gary Wang, M.D., Ph.D., an assistant professor of infectious diseases in the UF College of Medicine, and principal investigator of the study. “The whole idea is to be able to understand the microbial signature early — before patients develop disease. That could lead to development of novel molecular tools and biomarkers to screen for disease.”
Estimates vary widely, but up to two-thirds of people who have HIV also have periodontitis, according to a literature review in the journal Periodontology 2000. For patients whose immune system is compromised, periodontitis further contributes to poor health by hindering proper nutrition. It also affects the ability to derive pleasure from eating.
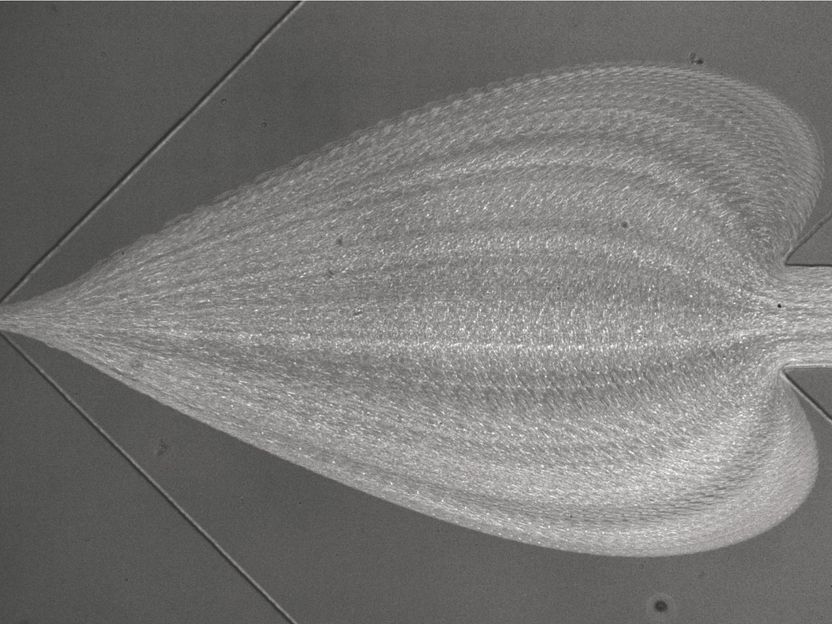
About 500 to 700 different species of oral microorganisms have been identified, and one person can have up to 100 different species in the mouth. In most cases those bacteria do no harm, and may in fact provide benefit by crowding out disease-causing bacteria. Communities of bacteria thrive in a thin film on the teeth, with different types of organisms clustering together into neighborhoods based on mutual benefit.
“There’s really not a place for an opportunist pathogen to get a foothold,” said Clay Walker, Ph.D., a professor of oral biology in the UF College of Dentistry and co-investigator in the study.
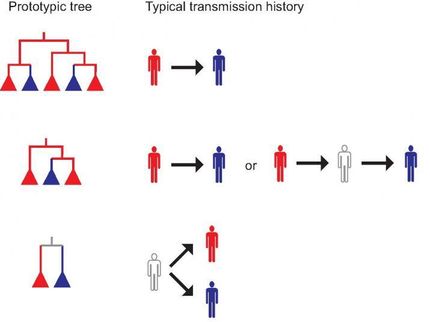
But when the immune response is compromised, as in HIV-infected patients, a shift in the composition of microorganism communities can allow opportunistic pathogens to grow freely. The UF team will examine those changes through a pilot study of HIV-positive and HIV-negative individuals who have chronic periodontitis.
The work is being carried out in collaboration with the Periodontal Disease Research Center, whose director is study co-investigator Nils Ingvar Magnusson, D.D.S., Odont. Dr., a professor of oral biology in the College of Dentistry.
The researchers will use sophisticated DNA sequencing techniques and bioinformatics to classify bacteria and identify differences between those in the two groups of patients. They also plan to track how bacterial composition in the mouth changes as people’s immune status changes.
“We’re interested in getting a definitive answer on whether there are differences in the bacteria associated with periodontitis in patients with HIV and in patients without HIV,” Walker said.
Previous analyses comparing periodontitis in people with HIV and in people without HIV have found no difference in the bacterial composition in the mouth. But today there are more sensitive molecular tools that have much greater ability to detect subtle differences.
A better knowledge of the microbe population in the mouth would enable the design of antimicrobials that are active against particular species of pathogens.
“If we do find that there are differences between the two, we may be able to use specific treatments to shift the flora or eliminate certain segments that may not be beneficial,” Walker said.
Most read news
Organizations
Other news from the department science

Get the life science industry in your inbox
By submitting this form you agree that LUMITOS AG will send you the newsletter(s) selected above by email. Your data will not be passed on to third parties. Your data will be stored and processed in accordance with our data protection regulations. LUMITOS may contact you by email for the purpose of advertising or market and opinion surveys. You can revoke your consent at any time without giving reasons to LUMITOS AG, Ernst-Augustin-Str. 2, 12489 Berlin, Germany or by e-mail at revoke@lumitos.com with effect for the future. In addition, each email contains a link to unsubscribe from the corresponding newsletter.
Most read news
More news from our other portals
Last viewed contents
Gene therapy start-up VectorY and Wageningen University sign strategic collaboration - Two-part project to develop novel baculovirus genome seeds and bioprocess technologies for the scalable production of AAV gene therapies
Curie-Cancer and Harmonic Pharma sign a partnership agreement for exploring the anti-cancer activity of several compounds