A decade of refinements in marrow and stem cell transplantation improves long-term survival of blood cancers
A decade of refinements in marrow and stem cell transplantation to treat blood cancers significantly reduced the risk of treatment-related complications and death, according to an institutional self-analysis of transplant-patient outcomes conducted at Fred Hutchinson Cancer Research Center.
Among the major findings of the study, which compared transplant-patient outcomes in the mid-‘90s with those a decade later: After adjusting for factors known to be associated with outcome, the researchers observed a statistically significant 60 percent reduction in the risk of death within 200 days of transplant and a 41 percent reduction in the risk of overall mortality at any time after transplant.
“Everything we looked at improved a decade after the initial analysis,” said George McDonald, M.D., a Hutchinson Center gastroenterologist and corresponding author of the paper, which was published Nov. 25, 2010 in the New England Journal of Medicine.
McDonald and colleagues reviewed the outcomes of 1,418 transplant patients who received peripheral-blood stem cells or bone marrow from unrelated donors between 1993 and 1997 and compared them to 1,148 patients who had the same procedures between 2003 and 2007. The malignancies treated included forms of leukemia, lymphoma, multiple myeloma and myelodysplastic syndrome.
The researchers also found that the estimated one-year overall survival rates for both groups were 55 percent and 70 percent, respectively. They also observed statistically significant declines in the risks of severe graft-vs-host-disease; infections caused by viruses, bacteria and fungi; and complications caused by damage to the lungs, kidney and liver.
Lead author and biostatistician Ted Gooley, Ph.D., noted that the analysis presents the findings in terms of the changes in the “risk” or “hazard” of death and transplant complications after taking into account the fact that the patients treated in the mid-2000s were, on average, older and sicker than those who were treated in the mid-1990s.
McDonald said he and his colleagues can only speculate about the reasons for the improved outcomes because the study was retrospective and was not a randomized comparison of transplant techniques and treatments among groups of patients. However, the authors deemed several changes in clinical practices to be important in risk reduction, many of which were the result of ongoing clinical research (including various randomized clinical trials) conducted at the Hutchinson Center and at other major transplant centers around the world:
- Careful pharmacologic monitoring and dose adjustments to avoid under and over treatment with the potent chemotherapeutic agents used in transplantation.
- Use of reduced-intensity conditioning in older and less healthy patients.
- Less use of high-dose systemic immune suppression to treat acute GVHD.
- Use of the drug ursodiol to prevent liver complications.
- New methods for early detection of viral and fungal infections as well as preventive therapy for such infections.
- The use of better and less toxic anti-fungal drugs to treat serious infections caused by Candidal organisms and molds.
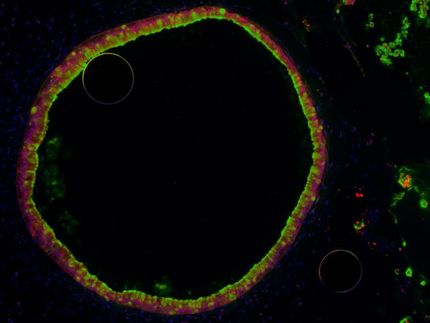
- Use of donor peripheral blood hematopoietic cells instead of bone marrow as the source of donor cells, which results in faster engraftment and return of immunity.
- More accurate matching of marrow or stem cell donors with unrelated patients.
“This research and the improved outcomes are the result of a team approach to one of the most complex procedures in medicine,” McDonald said. Medical oncologists and transplantation biologists at the Hutchinson Center are supported in the care of patients by specialists in infectious diseases, pulmonary and critical care medicine, nephrology, gastroenterology and hepatology, and by highly skilled nurses and support staff.
“Each of these programs is involved in ongoing clinical research into the complications of transplant, which results in constant changes in how transplantation is carried out,” he said. “These data show clearly that our collective efforts have improved the chances of long-term survival for our patients.”