UF discovery could lead to better genetic screening for diabetes
University of Florida researchers have identified a protein that affects how much insulin the body produces in people with a hereditary form of diabetes. Called maturity onset diabetes of the young, or MODY, the disease can be difficult to detect and is sometimes misdiagnosed as the more common type 1or type 2 forms of diabetes, in part because doctors have not been looking at the full genetic picture, said Li-Jun Yang, M.D., an associate professor of pathology, immunology and laboratory medicine in the UF College of Medicine.
If the disease has not been diagnosed, children with MODY are often treated with insulin injections like type 1 diabetes patients. The problem is, they don’t need to be. Instead of insulin injections — which can be dangerous if not administered precisely throughout the day — patients with the most common form of MODY can take a pill that stimulates insulin production to treat their disease.
“The clinical treatment for MODY can be so simple if you diagnose the disease accurately,” said Yang, the senior author of the study, which was published in the Journal of Biological Chemistry. “People will treat this either as type 1 or type 2, but that is not the best approach for managing this condition. That is why we think what we have discovered is so important.”
Nine forms of MODY have been identified, and each one is related to a mutation on a specific gene involved in insulin production. UF researchers studied MODY 3, the most common type, which affects about three-fourths of patients with the disease. But to accurately screen for it, experts have to know exactly where the genetic mutation occurs. Scientists know that MODY 3 is related to a mutation on a gene called hepatic nuclear factor 1-alpha. But currently, tests only scan part of that gene for errors.
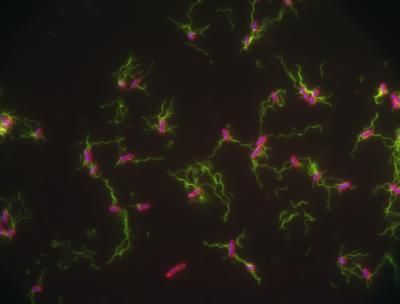
HNF1-alpha is just one of many genes that affect how much insulin the body produces. But even the gene itself is just one player in the game. Think of insulin production like a baseball game. The gene HNF1-alpha would be sort of like a pitcher, except instead of throwing a ball to home plate, it allows cells in the pancreas to produce insulin. And just like a pitcher, genes have coaches that tell them what to do. Only instead of chubby men in caps, a gene’s coach comes in the form of proteins that attach themselves to the gene and flip the on/off switch.
Researchers in Yang’s lab began hunting for proteins that could affect the gene with no luck, says William Donelan, a doctoral student in the College of Medicine and the first author of the paper. They had one sample left to test, a key protein named NKx6.1 — it turned out to be the coach.
“We had just about given up. We had tried lots of experiments looking for binding sites for these genes and nothing was working. This was the last one we tested out, and we had this huge spike in activity. We couldn’t believe it,” Donelan said. “I thought I did something wrong.”
Further testing in mouse cells showed that this protein was what Yang describes as a “key controller” for HNF1-alpha, the gene linked to MODY 3. Part of the reason for the lag in insulin production could be that the protein itself is mutated and not working, or it could be sending the wrong signals to the gene when it attaches.
“The current paper is a step forward in increasing the sensitivity of the screening for this form of diabetes because it has identified another important region that can be mutated and be the cause of diabetes,” said Alessandro Doria, M.D., an associate professor of medicine at Harvard Medical School and an investigator with Harvard’s Joslin Diabetes Center who studies MODY.
Unlike patients with type 1 diabetes, whose bodies attack and destroy their own insulin-producing beta cells in the pancreas, patients with MODY have perfectly healthy beta cells, Yang says. Patients with MODY 3 can take a drug that bypasses the genetic malfunction and triggers the body to produce insulin again.