How Immune Cells “Sniff Out” Pathogens
Researchers are using an innovative method to watch immune receptors go about their business
immune cells are capable of detecting infections just like a sniffer dog, using special sensors known as toll-like receptors, or TLRs for short. But what signals activate TLRs, and what is the relationship between the scale and nature of this activation and the substance being detected? In a recent study, researchers from the University of Bonn and the University Hospital Bonn (UKB) used an innovative method to answer these questions. The approach that they took might help to speed up the search for drugs to combat infectious diseases, cancer, diabetes or dementia. Their findings have been published in the journal “Nature Communications.”
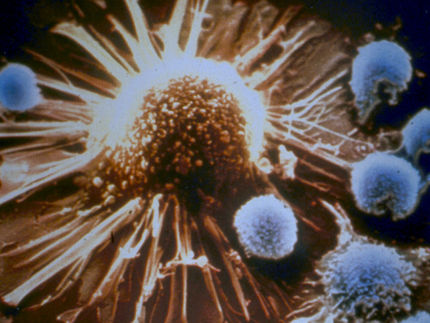
TLRs are found in great numbers on the surface of many of our cells, particularly those in the mucous membranes and those of our immune system. They work like the olfactory receptors in our nose, being activated when they encounter a specific chemical signal. The alarm that they trigger starts a series of reactions inside the cells. When scavenger cells “sniff out” a bacterium, for instance, they initiate a process known as phagocytosis by engulfing and digesting it, while other immune cells release special messengers that call for reinforcements and thus provoke inflammation.
TLRs activated by danger signals
There are several groups of TLRs, each of which responds to different “smells.” “These are molecules that have crystallized into important danger signals over the course of evolution,” explains Professor Günther Weindl from the Pharmaceutical Institute at the University of Bonn. Among them are lipopolysaccharides (LPS), which form integral parts of a bacterium’s cell wall.
“What we don’t yet know for certain in many cases is what responses are prompted by a signal being detected,” says Weindl, who is also a member of the Transdisciplinary Research Areas (TRAs) “Life & Health” and “Sustainable Futures”. “For instance, it’s quite possible that different molecules stimulate the same TLR but trigger different responses.”
Researchers usually attempt to answer this question by marking molecules in a different color, which tells them, for example, when the receptor switches on a certain signaling pathway in which these molecules play an important role. However, this method is very time-consuming and laborious and requires the observer to be very familiar with the signaling pathways already.
“Instead, we trialled a different technique that doesn’t require any color-coding and that’s already been used successfully to shed light on how other receptors work,” Weindl reveals. “We’ve now used this method for the first time to study TLRs.” The process is based on the fact that cells tend to change their form when they come into contact with a signal molecule in order, for example, to gear themselves up to “swallow” a bacterium or transform into infected tissue.
Changing the wavelength to make TLR activation visible
This change of form can be seen very easily by placing the cells on a specially coated transparent plate and shining a broadband light source on them from below. Certain regions (wavelengths) of the light spectrum are reflected where the light meets the coating—which ones in particular will depend on the processes and changes under way inside the cell.
“We were able to demonstrate that these changes in the reflected wavelengths kick in just a few minutes after adding the signal molecule,” says Weindl’s colleague Dr. Janine Holze. “We also brought cells into contact with E. coli and Salmonella lipopolysaccharides. Although both components of the cell wall stimulate the same TLR, the reflected spectrum changed in a different way after introducing the E. coli LPS than after adding their Salmonella counterparts.” This suggests that the same receptor is activated by different molecules in different ways and then triggers specific responses depending on the signal.
Says Weindl: “This method thus permits a much more nuanced explanation than before of how the receptors work as well as simplifying the search for potential drugs with a highly specific profile of action.” Possible uses include strengthening the immune response so that the body’s own defense forces can fight cancer cells more effectively. With diseases such as diabetes, rheumatism or Alzheimer’s, by contrast, the aim is to weaken specific aspects of the immune response that could otherwise damage healthy tissue, and the new method may well take researchers one step further toward this goal.