Leveraging intercellular mitochondria transfer to boost cancer immunotherapies
A new cancer busting platform
Advertisement
An international team of researchers, led by Professor Luca Gattinoni at the Leibniz Institute for Immunotherapy (LIT), has developed an innovative mitochondrial transfer platform to supercharge CD8+ T cells, enabling them to overcome exhaustion and more effectively fight tumor cells.
Cancer immunotherapies, which harness a patient’s immune system to target cancer cells, are revolutionizing the way we treat patients. Immune cells can locate and attack tumors in various ways and adapt to their environment. However, as “living drugs”, immune cells can run out of fuel and become exhausted, losing their ability to fight cancer. Mitochondria, the cell's primary energy sources, are crucial for maintaining immune cell function, and their loss or dysfunction is tightly linked to immune cell exhaustion. Emerging research has shown that mitochondria are not fixed but can move between cells restoring energy, altering cell behavior, and extending cell lifespan.
Mitochondrial transfer as a new cancer busting platform
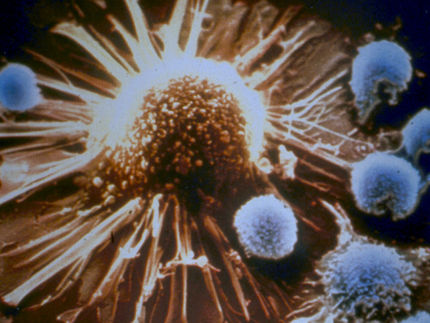
In a new study published in Cell, Professor Gattinoni’s team discovered that mitochondrial transfer occurs between bone marrow stromal cells (BMSCs) and T cells, the functional arm of the immune system responsible for clearing cancerous and infected cells. High-resolution imaging showed mitochondria travel through tiny tunnels called nanotubes, forming a bridge between the cells. T cells that received donor mitochondria became supercharged, expanded more robustly, infiltrated the tumor more efficiently, and showed fewer signs of exhaustion compared to T cells that did not take up mitochondria.
“Mitochondrial transfer as a technology platform is unique because rather than targeting a single specific gene or pathway to improve mitochondria within cells, we transfer whole intact mitochondrial organelles. This process is akin to organ transplantation –such as heart, liver, kidney transplants– but occurs at a microscopic level, involving the transfer of organelles between cells to enhance their function” explains Dr. Jeremy Baldwin, lead researcher on the paper. “It was exciting to see that this single approach could address many of the current challenges limiting the effectiveness of T cell therapies, such as poor T cell expansion, insufficient persistence, inadequate tumor infiltration, and the lack of sustained antitumor function,” adds Prof. Luca Gattinoni.
The team successfully applied their mitochondrial transfer technique across a broad range of T cell therapy platforms, including CAR and TCR-modified T cells, as well as tumor-infiltrating lymphocytes (TILs). “We previously observed that cancer cells can evade immune cell attacks by hijacking mitochondria from immune cells. Now, we show that we can counteract this by exploiting mitochondrial transfer for therapeutic purposes” comments Prof. Shiladitya Sengupta from Harvard University, co-corresponding author of the paper.
A long journey bears fruits of research
Prof. Luca Gattinoni began this research journey during his time at the National Cancer Institute (NCI) after being awarded an NCI Flex award in 2016 to explore the phenomena of mitochondria transfer to immune cells and he continued pushing this bold project forward when he moved his laboratory to the LIT in Germany with the generous support of Clinic & Laboratory Integration Program (CLIP) from the Cancer Research Institute (CRI). “I cannot express into words the rewarding feeling of watching your research evolve over the years, from the initial discovery under the microscope providing evidence of transfer to seeing its development into real-world applications” remarks Prof. Luca Gattinoni. Research however is not performed in isolation and the project involved many collaborators from leading institutes across the globe (including National Institutes of Health (NIH), Harvard University, San Raffaele University, ETH Zürich and FAU Erlangen-Nürnberg) all leveraging their unique skills and core competencies to achieve the research objectives.
What Are the Next Steps?
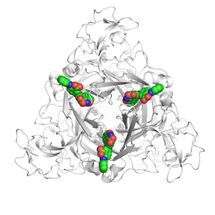
Future work will focus on scaling up the technology to clinically relevant cell doses. The team has already begun identifying key factors regulating mitochondrial transfer, such as Talin 2, a molecule involved in forming the tiny bridges that connect cells. Additional efforts will include finding a surrogate marker for label-free cell enrichment and identifying BMSC subsets, “Super Donors”, that are primarily responsible for mitochondrial transfer. “This discovery is rapidly changing our fundamental understanding of biological systems. I’m excited to see where the field progresses and how we can use these processes to benefit patients,” concludes Prof. Philipp Beckhove, scientific director of the LIT and contributor to the study
Original publication
Jeremy G. Baldwin, Christoph Heuser-Loy, Tanmoy Saha, Roland C. Schelker, Dragana Slavkovic-Lukic, Nicholas Strieder, Inmaculada Hernandez-Lopez,... Jacob E. Corn, Matteo Iannacone, Donato Inverso, Michael Rehli, Jessica Fioravanti, Shiladitya Sengupta, Luca Gattinoni; "Intercellular nanotube-mediated mitochondrial transfer enhances T cell metabolic fitness and antitumor efficacy"; Cell