Epigenetic changes reprogram astrocytes into brain stem cells
Discovery shows that astrocytes could potentially be used in regenerative medicine to replace damaged nerve cells
Advertisement
Resting brain stem cells hardly differ from normal astrocytes, which support the nerve cells in the brain. How can almost identical cells perform such different functions? The key lies in the methylation of their genetic material, which gives these special astrocytes stem cell properties. Scientists from the German Cancer Research Center (DKFZ) and Heidelberg University have published their findings in the journal Nature. In mice, the researchers showed that experimentally induced lack of blood flow in the brain epigenetically reprograms astrocytes into brain stem cells, which in turn can give rise to nerve progenitor cells. This discovery shows that astrocytes could potentially be used in regenerative medicine to replace damaged nerve cells.
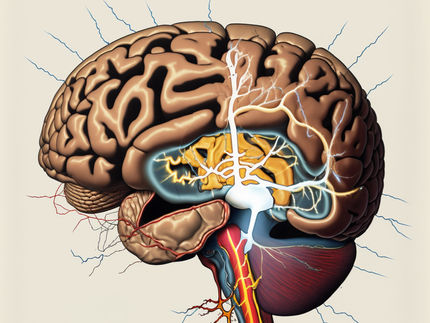
Many different types of cells work together in the brain. In humans, nerve cells (neurons) make up less than half of the cells. The rest are called "glia". The most common glial cells are astrocytes. They supply the neurons with energy, form part of the blood-brain barrier, regulate the synapses and support the immune cells.
However, a small proportion of astrocytes are able to produce nerve cells and other types of brain cells. These special astrocytes are therefore also known as brain stem cells. Brain stem cells and ordinary astrocytes hardly differ in their gene expression, i.e. in the activity of their genes. "How they can perform such different functions and what makes up the stem cell properties was previously completely unclear," explains Ana Martin-Villalba, stem cell researcher at the DKFZ.
Methylation is the key
To solve this puzzle, the teams led by Martin-Villalba and Simon Anders (BioQuant, Center, Heidelberg University) isolated both ordinary astrocytes and brain stem cells from one of the regions of the brain where young neurons develop in adult mice, the "ventricular-subventricular zone" (vSVZ). The researchers analyzed gene expression at the level of individual cells using mRNA sequencing as well as the patterns of methylation ("methylome") in the entire genome. They used a specially developed tool to analyze the methylation data*.
DNA methylation refers to chemical "markers" with which the cell can switch off unused parts of its DNA. Methylation is therefore crucial for the identity of the cells.
During this study, the stem cell experts noticed that brain stem cells have a special DNA methylation pattern that distinguishes them from other astrocytes. "Unlike normal astrocytes, certain genes are demethylated in brain stem cells that are otherwise only used by nerve precursor cells. This allows the brain stem cells to activate these genes in order to produce nerve cells themselves," explains Lukas Kremer, first author of the current publication. Co-first author Santiago Cerrizuela adds: "This pathway is denied to ordinary astrocytes, as the required genes are blocked by DNA methylation."
Lack of blood supply triggers reprogramming of astrocytes to stem cells and increases new nerve formation
Could methylation also be used to convert astrocytes into brain stem cells in other regions of the brain, outside the vSVZ? "This would be an important step for regenerative medicine to repair damaged areas of the brain," says Ana Martin-Villalba.
Earlier studies had already shown that a lack of blood supply, such as occurs in brain injuries, increases the number of newborn nerve cells. Do altered methylation profiles play a role in this process?
To investigate this, the researchers interrupted the blood supply to the brain of mice for a short time. As a result, astrocytes with the typical stem cell methylation profile could also be detected outside the vSVZ, as well as an increased number of nerve progenitor cells.
"Our theory is that normal astrocytes in the healthy brain do not form nerve cells because their methylation pattern prevents them from doing so," explains study head Martin-Villalba. "Techniques to specifically alter the methylation profile could represent a new therapeutic approach to generate new neurons and treat nerve diseases."
"The lack of blood flow apparently causes astrocytes in certain areas of the brain to redistribute the methyl marks on their DNA in such a way that their stem cell program becomes accessible. The reprogrammed cells then begin to divide and form precursors for new neurons," summarizes Simon Anders and adds: "If we understand these processes better, we may be able to specifically stimulate the formation of new neurons in the future. For example, after a stroke, we could strengthen the brain's self-healing powers, which normally just don't seem to be sufficiently active, so that the damage can be repaired".