Prostate cancer: AI should help to avoid unnecessary biopsies
For which men is a biopsy necessary to confirm or rule out suspected prostate cancer if the PSA value is elevated? In a retrospective study, scientists from the German cancer research Center (DKFZ) and the Department of Urology at Heidelberg University Hospital have shown that the combination of risk markers, systematic evaluation of MRI images and artificial intelligence (AI) can predict the risk of prostate cancer more accurately than before. In men with a low risk, it may not be necessary to remove tissue.
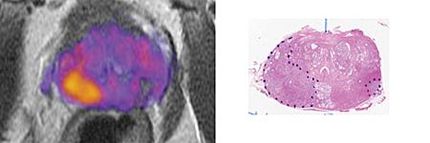
If a PSA test shows an elevated value, this may be an indication of prostate cancer. In order to clarify this suspicion, doctors today first order magnetic resonance (MR) imaging as further diagnostics. The "multiparametric MRI" used here combines various imaging techniques and therefore provides very detailed images.
However, final certainty can only be obtained by removing tissue from the prostate. "The biopsy is invasive and can, in rare cases, lead to infections or bleeding, sometimes even requiring hospitalization," says David Bonekamp, radiologist at the DKFZ. Doctors are therefore urgently looking for ways to improve risk prediction. "Our aim is to filter out those men who only have a minimal risk of cancer. They could be spared tissue removal or postpone it for some time. Men with a high probability of prostate cancer, on the other hand, benefit from the biopsy, as the cancer can be detected early," says Bonekamp.
Today, researchers use a calculator to estimate the risk of cancer, which takes into account various parameters such as PSA value, age and prostate volume as well as the MRI findings. To this end, doctors use a system known as PI-RADS for the systematized evaluation of MRI images, which ultimately provides a probability value for the presence of prostate cancer.
Could an AI based on deep learning further improve this prediction or possibly even replace PI-RADS? To test this, Bonekamp's team launched a retrospective study in which they included data from 1627 men who had undergone multi-parametric MRI imaging of the prostate in Heidelberg between 2014 and 2021 and subsequently underwent a biopsy.
An algorithm developed at the DKFZ for evaluating image data was trained with the MRI images of over 1000 of these men. Using the remaining 500 or so data sets, the researchers tested whether a combination of their risk calculator with the AI could improve the accuracy of prostate cancer prediction.
If the PI-RADS value in the risk calculator was replaced by the AI method, the diagnostic significance hardly changed. In contrast, the combination of AI and PI-RADS delivered significantly better results: It identified 49 percent as minimal risk among men who had originally been biopsied. "This means that the combination of deep learning and radiological findings could theoretically have avoided almost half of these biopsies without overlooking a relevant number of tumors," says Adrian Schrader from the DKFZ, first author of the current study.
The radiologists conclude from this result that deep learning-based AI and PI-RADS assessment by experienced radiologists evidently provide complementary diagnostic information, which together contribute to a more precise risk stratification of patients.
"For patients with an abnormal PSA value, integrating AI analysis into further diagnostics could be a great advantage in the future. However, prospective studies must confirm the benefits of the procedure and clarify that it has no disadvantages for patients," says Bonekamp.
Note: This article has been translated using a computer system without human intervention. LUMITOS offers these automatic translations to present a wider range of current news. Since this article has been translated with automatic translation, it is possible that it contains errors in vocabulary, syntax or grammar. The original article in German can be found here.
Original publication
Adrian Schrader, Nils Netzer, Thomas Hielscher, Magdalena Görtz, Kevin Sun Zhang, Viktoria Schütz, Albrecht Stenzinger, Markus Hohenfellner, Heinz-Peter Schlemmer, David Bonekamp; "Prostate cancer risk assessment and avoidance of prostate biopsies using fully automatic deep learning in prostate MRI: comparison to PI-RADS and integration with clinical data in nomograms"; European Radiology, 2024-7-2