HIV cured at Charité: the next Berlin patient
Team from Charité succeeds again in apparently fully eliminating HIV from a patient’s body
Advertisement
He went down in medical history: the “Berlin Patient,” the first person in the world to be cured of HIV, following a stem cell transplant at Charité – Universitätsmedizin Berlin. Now, a team from Charité has repeated this extremely rare medical achievement. The second Berlin patient has had no detectable virus for more than five years even though he is not taking antiviral medications. What makes this case special is that the team used a treatment method different from previous cases in which patients have been cured of HIV. It necessitates a new explanation of the mechanism by which the virus was cured.
Treatment for HIV has made huge strides. With good treatment, people living with HIV these days regularly experience a good quality of life. Even so, HIV is considered incurable – usually, that is. In extremely rare cases, stem cell transplantation has succeeded in eliminating the virus from the body.
Stem cell transplantation is only an option for patients who, in addition to living with HIV, also develop certain forms of leukemia or lymphoma that do not respond to radiation or chemotherapy alone. In this procedure, stem cells from a healthy person are transferred to the patient, in essence replacing the patient’s immune system. This makes it possible to fight not only the cancer, but also HIV. Scientists had previously believed it was necessary to find a stem cell donor with very specific genetic characteristics.
The role of the CCR5 receptor
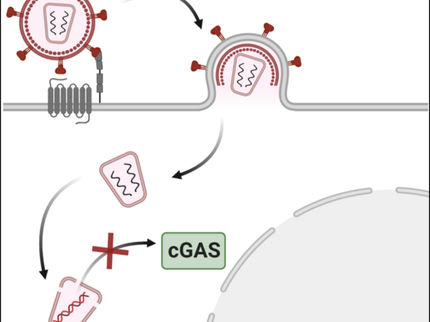
This is because in order to multiply, HIV enters various immune cells, which requires a certain type of receptor called the CCR5 receptor. About one percent of the European population has a CCR5 receptor with what is known as the delta 32 mutation. It prevents the virus from entering, making people with this mutation naturally immune to HIV. If it is possible to find a stem cell donor whose tissue is a match for the recipient and that person carries this immunity-causing mutation, then stem cell transplantation can cure not only the patient’s cancer, but also HIV.
A team from Charité demonstrated that this principle works back in 2008, when they applied it to the person who came to be known as the “Berlin Patient.” Since then, four more people worldwide have been treated in this way and are now viewed as having been cured of HIV. Now, Berlin’s university medicine organization has successfully treated a person with both acute myeloid leukemia (AML) and HIV a second time – albeit this time with a slightly different method. The case is to be presented to the medical world at the International AIDS Conference in Munich on July 24.
Treatment of the second Berlin patient
The patient, now 60, tested positive for HIV in 2009 and was additionally diagnosed with AML in 2015. A team from the Department of Hematology, Oncology and Cancer Immunology at Charité took him on as a leukemia patient. The patient’s risk profile meant that it was necessary for him to undergo both chemotherapy and additional stem cell transplantation.
“We couldn’t find a matching stem cell donor who was immune to HIV, but we did manage to find one whose cells have two versions of the CCR5 receptor: the normal one, and then an extra, mutated one,” explains Prof. Olaf Penack, a senior physician at the department treating the patient. “This occurs when a person inherits the delta 32 mutation from only one parent. However, having both versions of the receptor does not confer immunity to HIV.”
Even though the donor was not herself immune, it became apparent that the stem cell transplantation had been successful in curing HIV after the patient discontinued the recommended antiviral treatment on his own in 2018. The patient has been tracked very closely, and to date the treatment team has been unable to find any indication that the virus remains. The patient’s immune system is functional, and there are no detectable cancer cells, either. “We’re very pleased that the patient is in good health and doing well,” Penack says. “The fact that he has been under observation for more than five years and has been virus-free the whole time indicates that we did indeed succeed in completely eradicating HIV from the patient’s body. So we consider him cured of HIV.”
Cure despite the donor’s lack of HIV immunity
“It’s extremely surprising that the patient was cured even though the stem cell donor wasn’t immune to HIV,” says Prof. Christian Gaebler, an expert on HIV and research group leader at the Department of Infectious Diseases and Critical Care Medicine at Charité and the Berlin Institute of Health at Charité (BIH). He analyzed the case from the infectious disease perspective. “In previous stem cell transplantation cases involving donors who were not immune, the virus resumed replicating after a few months.”
The second Berlin patient proves that it is possible to cure HIV even though there is a functional receptor for the virus to use. “This means the fact that the virus was cured is apparently not attributable to the donor’s genetic CCR5 receptor, but instead to the fact that her transplanted immune cells eliminated all of the patient’s HIV-infected cells,” Gaebler explains. “By replacing his immune system, we apparently destroyed all the places where the virus was hiding, so it was no longer able to infect the new immune cells from the donor.”
What factors contributed to the cure?
Why stem cell transplantation led to the patient being cured in this case while the virus resumed replicating in comparable cases is still unclear. The researchers are considering multiple potential factors. “The speed at which the new immune system replaces the old one might play a part,” Gaebler says. “In the second Berlin patient, that was done relatively quickly, in less than 30 days. But the donor’s immune system might also have special characteristics, such as highly active natural killer cells, which ensure that even minor HIV activity is detected and eliminated.”
The researchers hope investigating the mechanism by which HIV has been cured in the second Berlin patient and potential additional cases will lead to new insights for future treatment of people with HIV. “Our goal remains to cure HIV not just in individual patients, but on a wider basis in the future,” Gaebler says. “But owing to the significant risks associated with stem cell transplantation, this method cannot be used as a standard treatment of HIV. Once we have a better understanding of which factors in the second Berlin patient contributed to the virus being eradicated from all its hiding places, then those findings can hopefully be used to develop novel treatment concepts such as cell-based immune therapies or therapeutic vaccines.”